Vesicoureteral reflux (VUR): causes, symptoms and treatment
Written in association with:In his latest online article, renowned consultant paediatric urologist and surgeon Mr Alex Turner explains the condition of vesicoureteral reflux (VUR) in detail. He explains the causes, symptoms and treatment options.
What is vesicoureteral reflux and what causes it?
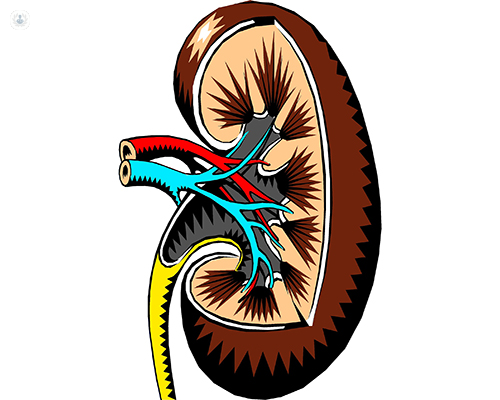
Vesicoureteral reflux (VUR) is a phenomenon in which the bladder squeezes to expel urine out of the urethra, but it also goes back up the ureters into the kidneys. Reflux can be primary or secondary. Primary reflux is more common.
Primary reflux is a very common condition. It is the leading cause of the requirement for renal replacement therapy in the UK, so it is quite a serious condition.
The ureters are tubes that travel from the kidney and insert into the bladder through a tunnel. This tunnel goes through a muscle. When the bladder squeezes during urination, the muscle pinches the tubes so urine cannot go back up the ureters.
However, for some children the tubes insert directly into the bladder. There is no tunnel and thus a defect in the muscle. This means that when the bladder squeezes, urine can easily go back up the ureters.
What are the symptoms patients with this condition experience?
Because urine goes back up towards the kidneys, this urine then trickles back down into the bladder. This means the bladder is never empty, with two effects:
- This puddle of urine is stagnant and can become infected. The infection can spread to the kidney and injure the organ.
- As the bladder doesn’t empty completely it gets confused. This means children with reflux can suffer from bedwetting or wetting themselves, as the bladder is never empty.

What are the treatment options for vesicoureteral reflux?
Patients will either present with an antenatal finding with a dilated renal tract, or they will present later with recurrent urinary tract infections. An ultrasound scan is mandatory to exclude reflux in investigations.
If there have been recurrent infections, something called a DMSA to look at scarring and the function of the kidneys will be done. The gold standard for detecting reflux is something called a micturating cystourethrogram (MCUG). This involves catheterising the bladder and putting dye into it to see on X-rays if it goes back up into the kidney.
The investigations we do will grade the reflux from 1 to 5, with 5 being the most serious. When we are considering treatment, we balance not only the grade of reflux but also whether there has been scarring and the holistic effects on the child.
The first treatment may be watching and waiting. This is considered if a child is well, with no infections or scarring and has low-grade reflux. Some children can even grow out of reflux.
However, in children who have recurrent infections and scarring, we first consider putting them on low-dose antibiotics to try and suppress the infection, before we consider the treatment.

The first thing we do is look in the bladder with a cystoscope. If the refluxing pipe is amenable to it, I can inject a substance into the mouth of the pipe to recreate the valve that is missing. This has variable success rates depending on the degree of reflux.
If this is not possible, or if it fails, then we need to consider a surgical procedure.
There are usually two options:
- A robotic approach, using keyhole surgery to replant the ureter. This creates a tunnel for the ureter.
- Open surgery is sometimes necessary, in which the bladder is opened and the ureter is reimplanted.
How is VUR related to urinary tract infections and kidney damage?
The puddle of urine in the bladder that is caused by reflux can easily become infected, and when this is refluxed up into the kidney again, it can cause kidney infections.
There is also the pressure effect on the kidney, especially the developing kidney in utero. This damages the nephrons, the tiny functioning units of the kidney, and can cause global or localised scarring of the infected kidney. This is why it is so important to investigate and treat it effectively.
Mr Alex Turner is a highly-experienced consultant paediatric urologist and surgeon based in Leeds. If you would like to book a consultation with Mr Turner, you can do so today via his Top Doctors profile.


