What's involved in an Arthroplasty?
Escrito por:Arthroplasty, also referred to joint replacement surgery, is a procedure where a damaged joint is replaced with an artificial implant.
Here to provide a detailed look at what’s involved in this procedure, is leading trauma and orthopaedic surgeon Mr Ricci Plastow.
What is an Arthroplasty?
This surgery is most often performed on the hip, knee, shoulder and elbow joints, but it can also be done on other joints. Arthroplasty is typically recommended for patients with severe joint pain or dysfunction caused by conditions such as osteoarthritis, rheumatoid arthritis or traumatic injury.
Preoperative assessment and preparation
Before undergoing Arthroplasty, patients will go through a thorough preoperative assessment to ensure they are fit for surgery. This assessment may include:
- Medical evaluation: A comprehensive review of the patient’s medical history, current health status and medications.
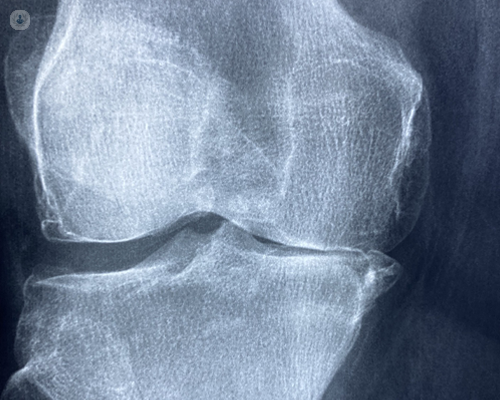
- Imaging studies: X-rays, MRI or CT scans to evaluate the extent of joint damage and plan the surgery.
- Laboratory tests: Blood tests to check for any underlying conditions that might affect the surgery or recovery.
- Consultation with a surgeon: Discussion of the surgical procedure, the type of implant to be used, and what to expect during recovery.
Patients are also advised to prepare for surgery by maintaining a healthy diet, quitting smoking, and discussing any medications they are taking with their healthcare provider.
What’s involved in the surgical procedure?
Arthroplasty is typically performed under general or regional anaesthesia, depending on the joint being replaced and the patient's medical condition. Here’s what happens during the procedure:
- Incision: The surgeon makes an incision over the affected joint to access the damaged area.
- Removal of damaged tissue: The damaged cartilage and bone are carefully removed from the joint.
- Implant placement: The surgeon then places the artificial implant, which is usually made of metal, ceramic or plastic. The implant is designed to replicate the movement and function of a healthy joint.
- Closure: Sutures or staples are used to close the incision. Then a sterile dressing is applied.
The surgery can take anywhere from one to several hours, depending on the complexity of the joint being replaced.
Postoperative care and rehabilitation
After surgery, patients will be closely monitored in a recovery room before being transferred to a hospital ward. Postoperative care is crucial to ensure a successful recovery and typically includes:
- Pain management: Medications are provided to manage pain and discomfort following surgery.
- Physical therapy: Early mobilisation is encouraged, often starting the day after surgery, to prevent complications such as blood clots and to promote healing. A physical therapist will guide the patient through exercises to strengthen the muscles around the new joint and restore range of motion.
- Wound care: Patients are advised on how to care for the surgical site to prevent infection.
- Follow-up appointments: Regular check-ups with the surgeon are scheduled to monitor the healing process and the function of the implant.
Most patients can expect to stay in the hospital for a few days following surgery, with a full recovery taking several weeks to months, depending on the joint replaced and the patient’s overall health.
What are the long-term outcomes with arthroplasty?
Arthroplasty is generally very successful, with most patients experiencing significant pain relief and improved joint function. The longevity of the implant varies but can last 15 to 20 years or longer, depending on factors such as the patient’s activity level, weight and the type of implant used. In some cases, a revision surgery may be needed if the implant wears out or fails.
In summary, Arthroplasty is a well-established surgical procedure that can significantly improve the quality of life for patients with severe joint pain or dysfunction. With proper preparation, skilled surgical intervention, and dedicated postoperative care, most patients can expect to return to their daily activities with greatly reduced pain and improved mobility.
Do you require an Knee arthroplasty? Arrange a consultation with Mr Plastow via his Top Doctors profile.


