All about the pacemaker fitting procedure
Written in association with:Here to tell us all about getting a pacemaker fitted is leading consultant cardiologist and electrophysiologist Dr Malcolm Finlay.
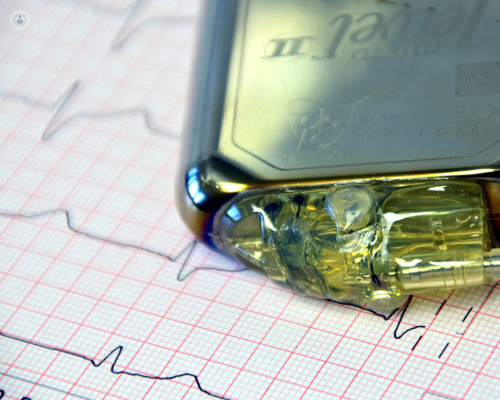
What are pacemakers?
These are small devices inserted under local anaesthesia in the shoulder just underneath the collarbone. They have one (“single chamber”) or two (“dual chamber”) wires (leads) that run to the heart and, in most circumstances, listen for the heartbeat and if the heart runs too slowly, they stimulate the heart to beat.
They are very good at preventing the heart from running too slowly. Sometimes we also use them so that patients can have a fast heart beat treated with medication or a procedure. Insertion of a pacemaker is a minor procedure, performed under local anaesthetic. It usually between 45 minutes and an hour, and people go home the same day of their procedure.
How long does it take to recover after having a pacemaker fitted?
After the procedure, it's normal to experience some discomfort or mild pain in the area where the pacemaker was inserted, but this usually subsides within a few days to a couple of weeks. Over-the-counter pain relief, such as paracetamol, is usually completely sufficient to manage this. I recommend avoiding rigorous movements or heavy lifting with the arm on the side of the pacemaker for about four to six weeks to allow the device and leads to settle securely. It's crucial not to strain the area or overextend your arm during this period, as this could disrupt the placement of the leads.
What aftercare is involved?
I use soluble sutures, and the wound will be well on the way to being completely healed within about a week, so I suggest keeping it dry for just that period (seven days). Your first follow-up appointment will typically be scheduled about four to six weeks after the procedure, with subsequent routine checks every six to 12 months or as recommended by your healthcare team. These check-ups are important to monitor the function of your pacemaker and to identify when the device might be nearing the end of its battery life.
Are there any risks involved in having a pacemaker fitted?
Of course, there is a risk to every medical procedure and this is no exception. A cut in the skin is made and bleeding or nasty bruising can occur. Serious complications that require further procedures occur in around one in 20 people having a pacemaker. This includes scratching the lung, which may require a drain (pneumothorax), and serious bleeding which may require a drain (pericardial or pleural bleeding). The pacemaker leads sometimes move which would require a second procedure to replace them or change their position.
The most serious risk is that of infection, and if this occurs the pacemaker must be removed for the infection to be treated. Thankfully this is rare, but occurs in approximately one in 200 patients. This is a major procedure with a one per cent mortality and often requires several weeks in hospital. Of course, everything is done to prevent this, including giving antibiotics before the procedure.
How long do pacemakers last for?
Pacemakers have a finite battery life and the generator must be changed after eight to 12 years depending on the current draw of the pacemaker. This is a minor, day case procedure, with similar risks to the initial implant.
There are now pacemakers available which are entirely implanted in the heart where the battery and device is miniaturised so that the entire pacemaker consists of a tiny, capsule-shaped device which goes into the pumping chamber of the heart. These are called “Micra™” pacemakers. These are ideal for some people, but for most, the standard type of pacemaker is best.
The procedure code for a standard dual-chamber pacemaker is: K6010. This has two leads to the heart and is the most suitable implant for you in my opinion. Most people who have a pacemaker performed as a booked procedure find they can return to their normal activities very quickly and enjoy a significantly improved quality of life.
If you require expert pacemaker surgery, arrange a consultation with Mr Finlay via his Top Doctors profile.


