All about vascular occlusions and their treatment
Written in association with:Leading consultant ophthalmologist Ms Lakshika Perera provides a detailed look at vascular occlusions and their treatment in this informative article.
What are vascular occlusions?
Vascular occlusions occur when blood flow to a specific area of the body is blocked or restricted due to the narrowing or blockage of blood vessels. In the context of ophthalmology, vascular occlusions refer to the obstruction of blood flow to the retina or optic nerve, leading to vision loss or other visual disturbances.
What causes vascular occlusions?
Vascular occlusions in the eye can be caused by various factors, including:
- Atherosclerosis: The buildup of fatty deposits (plaques) in the arteries, leading to narrowing or blockage of blood vessels.
- Blood clots: Formation of blood clots within the blood vessels, which can obstruct blood flow.
- Diabetes: Chronic high blood sugar levels can damage blood vessels and increase the risk of vascular occlusions.
- Hypertension: High blood pressure can damage the delicate blood vessels in the eye, increasing the risk of occlusions.
- Glaucoma: Increased intraocular pressure can compress blood vessels, leading to reduced blood flow to the optic nerve.
- Retinal artery or vein compression: Mechanical compression of retinal blood vessels by adjacent structures can impede blood flow.
How are vascular occlusions diagnosed?
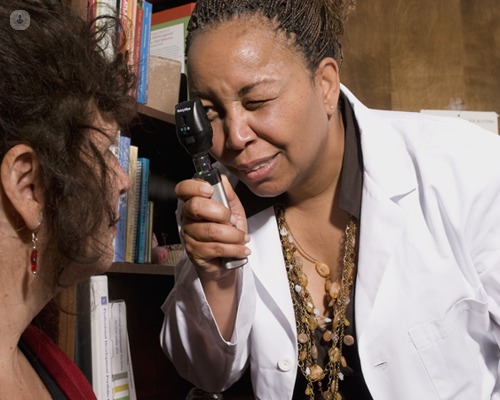
Vascular occlusions are typically diagnosed through a comprehensive eye examination by an ophthalmologist. Diagnostic tests may include:
- Fundus examination: Visualising the retina and optic nerve to assess for signs of vascular occlusions.
- Optical coherence tomography (OCT): Imaging technique to visualise the layers of the retina and detect abnormalities.
- Fluorescein angiography: Injection of a fluorescent dye into the bloodstream to visualise blood flow in the retina and identify areas of blockage or leakage.
- Visual field testing: Assessing the patient's peripheral vision to detect any visual field defects.
What are the treatment options for vascular occlusions?
Treatment for vascular occlusions aims to improve blood flow to the affected area and prevent further vision loss. Treatment options may include:
Intravitreal injections
Administration of anti-vascular endothelial growth factor (VEGF) medications or corticosteroids directly into the eye to reduce inflammation and promote blood vessel regression.
Laser photocoagulation
Use of laser energy to seal leaking blood vessels or create new blood vessel formation (neovascularisation) to bypass blocked vessels.
Retinal surgery
Surgical procedures such as vitrectomy or retinal artery/vein cannulation may be performed in cases of severe vascular occlusions to restore blood flow or remove obstructions.
Medications
Oral medications such as anticoagulants or antiplatelet agents may be prescribed to prevent blood clots and improve blood flow.
How serious are vascular occlusions?
The prognosis for patients with vascular occlusions varies depending on the severity of the condition and promptness of treatment. Early diagnosis and intervention can help preserve vision and prevent further vision loss. However, in some cases, vascular occlusions may lead to permanent vision impairment or blindness, especially if left untreated or if associated with underlying systemic conditions such as diabetes or hypertension.
Do you require expert treatment for vascular occlusions? Arrange a consultation via Ms Perera’s Top Doctors profile.


