An expert's guide to fertility preservation for gynaecological cancer
Written in association with:In the past, many women who had gynaecological cancer were unable to have children after treatment. However, in recent years many advancements have been made in the different treatments for this cancer, allowing for fertility preservation in some cases. In his latest article, renowned gynaecologist and gynaecological oncologist Mr Gautam Mehra explains how fertility is preserved in these certain cases.

What is fertility preservation?
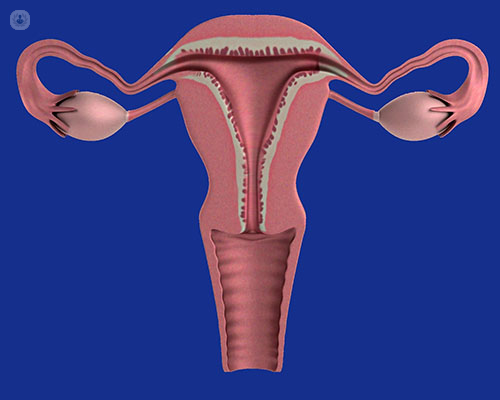
Fertility preservation is when surgery is done but the reproductive organs are left intact. This means the woman receiving treatment can still bear children.
How is it different for gynaecological cancer patients?
It is quite challenging when we have gynaecological cancer patients because cancer spreads and can progress. We can still preserve fertility in some cases of gynaecological cancers. For example, if you are young and have ovarian cancer that is still in the early stages, we can leave the other ovary behind and you will still be able to bear children.
Follow-up after surgery is extremely important as there is a small chance that some of the disease remains and will spread. In cervical cancer, sometimes we remove the cervix but leave the uterus, and some women can then conceive after surgery. The follow-ups after the surgery must continue to ensure that the cancer does not come back.

What are recent advancements in fertility preservation?
A lot of advancements have been made in the last two decades with regard to fertility preservation for gynaecological cancer patients. Previously, we had to do radical surgery and remove reproductive organs.
Now, fertility can be preserved in certain cases. One such treatment is trachelectomy, in which the cervix is removed but the uterus is kept. You can still get pregnant after this. Data from the past two decades has shown that this is safe and there is a good chance of getting pregnant following the procedure.
For ovarian tumours, we can sometimes preserve the other ovary and uterus which preserves fertility.
In endometrial cancer, we also have a treatment available that preserves fertility if the cancer is in its early stages. Outcomes for this procedure have been good overall. We try and work with assisted conception unit after surgery to ensure you can get pregnant.
Another new advancement is the use of cryopreservation. This is when an organ is removed and preserved, and reintroduced to the body later when you want to get pregnant.
How long can fertility preservation take from start to finish?
This depends on the treatment. Usually, after surgery to treat cancer, you will need to wait at least a couple of months to recover before trying to conceive. Usually, the advice given to cancer patients who want to have children in the future is to try and conceive as soon as possible. Sometimes we will even discuss the surgery in which we remove the uterus and other reproductive organs after they have completed their family.
Sometimes women will undergo chemotherapy after surgery, and this can negatively affect their fertility as well. We will work with the fertility specialist to try and give each patient the best chance of preserving their fertility.
How does life change afterwards?
This depends on the treatment you had. If the cervix is removed due to very early cancer, then there is not much that will change other than going to follow-ups to ensure the cancer hasn’t returned. If the whole cervix is removed, about 65 – 75% of women will be able to get pregnant. About 25% of these women will have pre-term labour, ad the baby will be delivered through caesarean section. This is because the neck of the uterus is closed with a stitch which retains the pregnancy in the uterus.
If you are having surgery for ovarian cancer, there is no change in what happens to you during life. Your other ovary will still work and allow you to get pregnant. Your follow-ups will still continue for at least 10 years as tumours can reoccur.
If you are receiving medical treatment for womb cancer where the womb has been preserved, we will wait for two negative biopsies following treatment before you can go to a fertility specialist to try and get pregnant.
Chemotherapy can hamper the function of the ovaries and may cause you to go through premature menopause. If a woman is to undergo chemotherapy, we will have a discussion about the possibility of preserving her eggs and embryos.
Mr Gautam Mehra is a renowned gynaecologist & gynaecological oncologist based in London. If you would like to book an appointment with Mr Gautam you can do so today on his Top Doctors profile.


