Complications in Reverse Total Shoulder Arthroplasty (RTSA)
Written in association with:Leading consultant orthopaedic shoulder and elbow surgeon Mr Paolo Consigliere expertly details how the potential complications in a reverse total shoulder arthroscopy procedure have significantly improved over recent times.
How have RTSA complication statistics improved?
Over the past 15 years, reverse total shoulder arthroplasty (RTSA) has undergone significant advancements, leading to a notable reduction in complications since the initial reports of the procedure. Initially, RTSA was associated with high rates of complications such as scapular notching, prosthetic loosening and infections, which posed considerable challenges for both patients and surgeons.
However, improvements in surgical techniques, prosthetic designs and postoperative care have substantially mitigated these risks. Recent studies indicate a decline in the incidence of these complications, highlighting the evolution of RTSA into a more reliable and effective treatment option for complex shoulder pathologies. This progress underscores the importance of continued innovation and research in enhancing patient outcomes and the overall success of RTSA.
Scapular notching
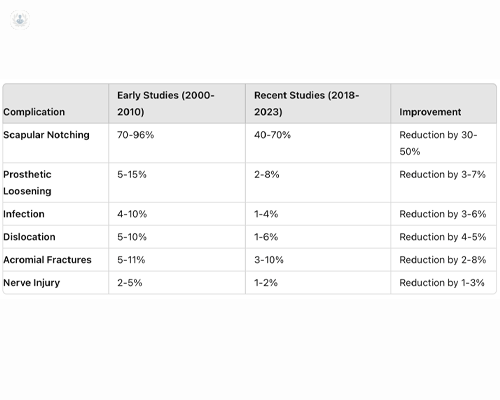
- Details: Scapular notching refers to the erosion of the scapular neck caused by impingement of the humeral component during shoulder movement. This complication can potentially lead to decreased range of motion and prosthetic wear.
- Early studies: Notching rates were alarmingly high, with reports indicating up to 96 per cent incidence due to poor implant design and surgical technique.
- Recent improvements: Advances in implant design and surgical approaches have reduced this rate to 40 to 70 per cent, demonstrating substantial progress in mitigating this complication.
Prosthetic loosening
- Details: Loosening of the prosthetic components, either the humeral or the glenoid, can lead to pain, instability, and the need for revision surgery.
- Early studies: Loosening was a common concern, with rates ranging from five to 15 per cent, often leading to the need for revision surgery.
- Recent improvements: Current reports indicate a loosening incidence of two to eight per cent, reflecting improved fixation techniques and material advancements.
Infection
- Details: Postoperative infections can occur superficially or deep within the joint, necessitating prolonged antibiotic therapy and sometimes additional surgeries.
- Early studies: Infection rates were concerning, reported between four to 10 per cent, raising significant postoperative risks.
- Recent improvements: Enhanced surgical protocols and antibiotic prophylaxis have lowered infection rates to one to four per cent, significantly improving patient safety.
Dislocation
- Details: Dislocation of the prosthesis can occur due to improper positioning of the components, soft tissue imbalance or trauma. This complication may require closed reduction or revision surgery.
- Early studies: Dislocation rates were found to be between five to 10 per cent, complicating postoperative recovery.
- Recent improvements: With refined surgical techniques, dislocation rates have dropped to one to six per cent, demonstrating enhanced stability of modern implants.
Acromial fractures
- Details: Fractures of the acromion or scapular spine can occur due to altered biomechanics and increased stress on these structures postoperatively. RTSA function relies on the increased tension of the deltoid muscle. This muscle inserts onto theacromion; excessive tension or poor bonce quality can result in a fracture. These are very difficult to treat and can lead to poor outcomes.
- Early studies: The incidence of acromial fractures was noted between five to 11 per cent, often linked to increased stress on the scapula.
- Recent improvements: The adoption of more lateralised designs in reverse total shoulder arthroplasty (RTSA) has significantly contributed to reducing the risk of acromial fractures. These designs enhance deltoid wrapping, which optimizes the biomechanical leverage of the deltoid muscle, distributing the mechanical load more evenly across the shoulder. This improved load distribution decreases stress concentrations on the acromion and scapular spine, thereby reducing the incidence of fractures in these regions, recently reported around three to 10 per cent.
Nerve injury
- Early studies: Nerve injuries were a significant concern, with rates of two to five per cent.
- Recent improvements: Ongoing refinement in surgical approaches has led to a decrease in nerve injury rates to one to two per cent, improving overall functional outcomes.
The evolution of reverse total shoulder arthroplasty over the last 15 years has led to marked improvements in complication rates. Continuous advancements in surgical techniques, implant design, and postoperative management have significantly enhanced patient outcomes, reinforcing RTSA as a reliable option for complex shoulder conditions.
If you’re looking for expert orthopaedic care, arrange a consultation with Mr Consigliere via his Top Doctors profile.


