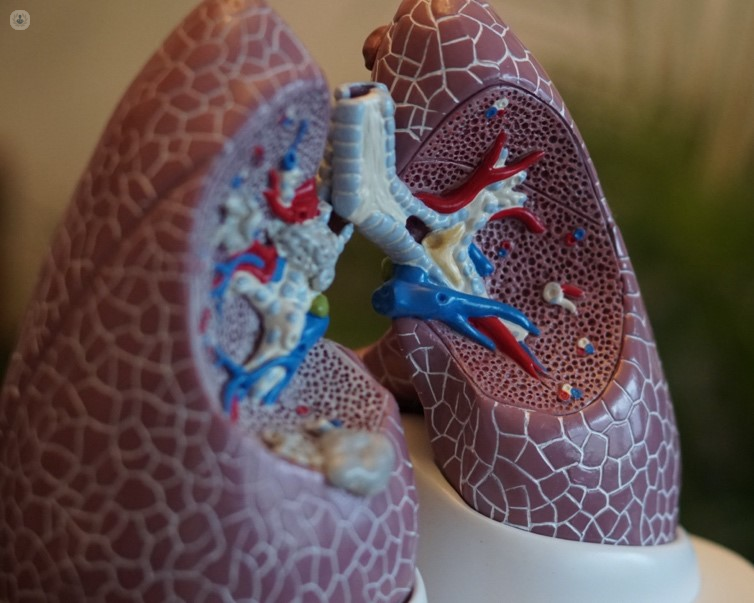
Coronavirus and lung issues
Written in association with:Most people who contract COVID-19 and test positive for the virus will develop mild to moderate symptoms, however, some may be severely impacted. With the ongoing pandemic affecting our daily lives, we wanted to learn how the situation is being managed and how we can lower the risk of the virus impacting our bodies.
We spoke with a leading specialist in pulmonology and respiratory medicine, Dr Grace Robinson, to discuss how COVID-19 can affect the lungs, the risk factors and how they can be mitigated.
Does the coronavirus always infect the lungs?
Yes, most people will have a cough and will present with respiratory symptoms.
What happens when the lungs are involved?
Typically, people will have a cough, feel breathless and have chest pain. For some, it will cause the lungs not to work well and they may need an oxygen concentrator. Those people need to come into the hospital for specific treatment.
What are the symptoms of COVID-19 when the lungs are affected?
Coughing, breathlessness and pain.
How can COVID damage the lungs?
It affects the lungs when the virus is there and people are acutely unwell, which is why people then feel breathless and are not able to transfer oxygen normally. Some will have scarring afterwards which is a tiny portion of people.
Who is at risk of COVID-19 lung complications?
Anyone who gets severe covid that affects the lungs. As we are well aware, old people, males, BAME communities, those with diabetes and obesity seem to be the main risk factors.
How should people reduce their risk?
Follow government guidance, such as ‘hand face space’, wear a mask, don’t leave your house unless it’s necessary, abide to social distancing and social isolation rules. We can reduce our risk by focusing on prevention.
Once you’ve got COVID-19 there’s not really much you can do to reduce its impact. The history of your health, age, weight, diabetes are the most influencing factors. However, when it comes to reducing the risk of the virus, there should be a primary focus on not getting the virus in the first place. It doesn’t matter which vaccine you have, they will all offer protection so when you’re offered it, have it.
If you require advice about symptoms you may have developed, phone a GP and get a test if necessary, isolate, as per the guidance that is widely available on the UK government website. If you have a cough, breathlessness or pain, seek an assessment from your GP or your local health service that may have a virtual ward. If you’re not too unwell you may still require some monitoring, you can be given an oximeter to have a phone call to assess oxygen levels and manage it at home remotely.
More unwell people need to be managed in hospitals. For example, if experiencing confusion (delirium) or diarrhoea. The older population are likely to have a respiratory illness as a result of COVID-19, steroids and antivirals may be given by the hospital. Critically ill patients may need additional treatment. Some people may need to be in the hospital for several weeks.
If you would like guidance regarding the health of your lungs, you may like to get in contact with an expert such as Dr Grace Robinson. Click here to visit her profile today to find out more information on appointment availability.


