COVID-19: is delirium a symptom of coronavirus?
Written in association with:During the global pandemic, there has been emerging evidence that shows delirium as a symptom found in coronavirus patients. Delirium is a well-recognised complication of respiratory illness in older adults and usually occurs in a patient who is already unwell with a lung condition, such as pneumonia.
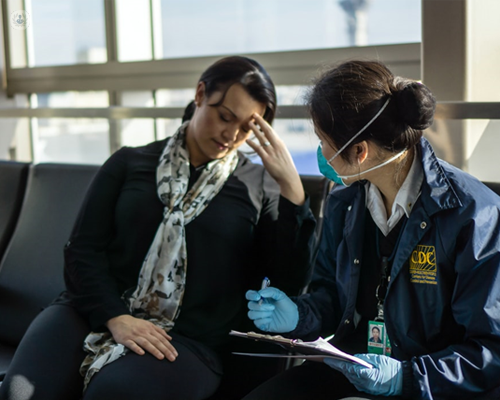
We may all be aware by now that dry cough, fever and difficulty in breathing are common signs of COVID-19, but is delirium an under-recognised symptom that people need to know about too? We spoke to one of our highly-acclaimed consultants in geriatric and general medicine, Dr Prashanth Reddy, about the link between coronavirus and delirium.
What is delirium?
Delirium is characterised by the following symptoms:
- Sudden confusion
- The inability to speak or think clearly
- A struggle to pay attention
- Hallucinations and delusions
- Reduced awareness
- Feelings of paranoia
- Reduced memory
Delirium can be categorised as hyperactive or hypoactive. The most recognised type is hyperactive delirium, which presents with symptoms of agitation and anxiety whereas hypoactive delirium is characterised by lethargy, sleepiness and confusion. The latter of the two is more common, however, many patients experience a combination of both types.
How does delirium tie into being a symptom of COVID-19?
Around 20 to 30% of those admitted to hospital who are critically ill present with features of delirium. People often think of coughing and difficulty in breathing as a diagnostic marker of COVID-19, but delirium is very common in cases of coronavirus.
If you or your loved one is showing signs of delirium, you need to get in touch with your healthcare professional immediately. Typically, delirium is associated with older patients but now we are seeing those who are younger become quite delirious with coronavirus.
The World Health Organization recognises that “altered consciousness and confusion” may be a presenting symptom of coronavirus in some patients even before fever and cough.
In other cases, a viral infection, such as coronavirus, and a symptom of fever may actually trigger delirium. The presence of pre-existing illnesses, such as high blood pressure, cardiovascular diseases, diabetes and pulmonary disease such as asthma, can also lead to the onset of an acute confusional state. Those who are admitted to the ICU are most at risk of developing delirium.
Is there any research on delirium and coronavirus?
I recently participated in a research study at the King’s College Hospital London with the Department of Clinical Gerontology, which collected data on 212 patients admitted to King’s between February and July 2020. This was linked with a national project known as CovidCollab, run by the Geriatric Medicine Research Collaborative.
In looking at patients with an age range of 70-97 (average age of 82), we found that half of these patients were diagnosed with delirium during their hospital admission. In those who presented to the hospital with delirium, however, we found that 39% had a fever and 47% had cough and shortness of breath.
This highlights how delirium is a common presenting symptom of COVID-19 and it also often occurs without the other classical symptoms of the disease.
How long does delirium last?
The duration of delirium is variable. The onset of the condition is usually abrupt and can last for hours or even days. In some people, it can last for weeks, for others months.
How can doctors prevent delirium in COVID-19 patients?
Delirium can be prevented in some cases and can be managed if your healthcare provider implements the following:
- They look for and treat all causes of delirium, such as constipation and dehydration.
- They encourage family members to monitor and report on behaviour that might indicate signs of delirium.
- Family members can help in providing gentle reorientation, such as reminding the patient what day it is and where the patient is.
- Patients should eat an adequate diet and drink plenty of fluids.
- Doctors should avoid sedating coronavirus patients as much as possible.
- Patients should be as active as possible rather than staying in bed.
What are the long-term consequences of delirium and COVID-19?
We don’t know and this is yet to be determined. We have seen that people have prolonged delirium for up to three to four months after having COVID-19 and that they haven’t gone back to normal. We know that it lasts longer than other types of delirium. The UK government is currently* working alongside specialists to set up rehab units for those with prolonged delirium.
How do you manage patients with delirium and COVID-19?
People who live with dementia are at a higher risk of delirium and they should have an assessment with a specialist such as myself. During the pandemic, they should be more careful, practice hygiene and follow the isolation regulations that have been suggested by the government.
Dr Reddy is a specialist in treating Parkinson’s disease, restless leg syndrome, dementia and osteoporosis. At the moment, he is available for a face-to-face appointment and also via video call using our e-Consultation tool. Book an appointment via his Top Doctor’s profile here.
**The information about COVID-19 in this article is subject to change from the date it was originally published.



