Diabetic retinopathy: An expert's guide
Written in association with:Mrs Samantha Mann is a leading consultant ophthalmologist based in London. In her latest article, Mrs Mann explains diabetic retinopathy in detail, including why it occurs and the best treatment.
What part of the eye can be affected by diabetes?
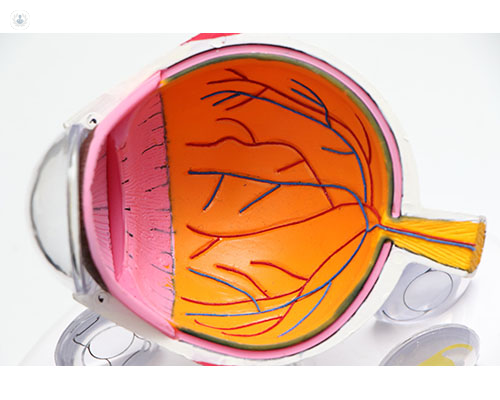
Diabetes predominantly affects the retina at the back of the eye. The retina is the very thin film on the inner surface of the eye that allows us to see. After having diabetes for a number of years or if the diabetes is poorly controlled, the blood supply can slowly reduce at the back of the eye. This results in the release of growth factors that can cause abnormal blood vessels to grow. The blood vessels can sometimes bleed and affect your vision, but this can be treated if caught early enough.
Additionally, small blood vessels can leak towards the centre part of the back of the eye, causing swelling of the macula to occur. This can also affect vision if left untreated.
How does diabetic retinopathy occur?
Increased blood sugar over a period of time causes changes to the walls of the blood vessels and blood cells. These changes affect the blood supply at the back of the eye, releasing growth factors which can cause diabetic changes on the retina such as haemorrhages and changes to the veins.
Eventually, abnormal blood vessels can grow on the surface of the retina which can bleed into the eye causing problems with vision. Treatment can often prevent this bleeding from occurring if caught early enough.
Additionally, small blood vessels can leak towards the centre part of the back of the eye causing swelling and blurred vision in advanced cases. Again, this can be treated to reduce the risk of sight loss.

How can you tell if diabetes is affecting your eyes?
Often the early signs of retinopathy do not have any symptoms. It is important to have your eyes checked or screened every year if you have diabetes. Once retinopathy progresses to the advanced stages you may get symptoms of black floaters in the vision or blurred vision.
How long does it take for diabetes to damage the eyes?
It can take several years for diabetes to damage the eyes. If diabetes is diagnosed late or the control is poor, the changes can come on much more quickly.
Can diabetic retinopathy go away without treatment?
Diabetic retinopathy is a progressive condition and so is unlikely to go away without treatment. If diabetic control is improved along with blood pressure and cholesterol control, some reversal of early changes is possible. Also, good diabetic control can slow the progression of retinopathy over time.

What is the best treatment for diabetic retinopathy?
This depends on which part of the retina is affected. In the early stages of retinopathy, observation and good diabetic control are all that are needed.
If the retinopathy progresses to the more advanced stages with abnormal blood vessel growth, the current best-recommended treatment remains Pan-retinal laser treatment. This treatment can shrink abnormal blood vessels and reduce their risk of bleeding. Once bleeding occurs, however, a surgical procedure, called a vitrectomy, may be required.
If diabetes has affected the central part of the retina, causing swelling, other treatments may be recommended. Observation can be the best treatment in the early stages, or if the swelling increases, laser or injection treatments may be required.
The injection treatments have to be given regularly but are very effective at reducing the swelling at the back of the eye and can restore vision if blurring has occurred. These treatments can be given quickly and safely into the eye with minimal discomfort.
Mrs Samantha Mann is a leading consultant ophthalmologist with over 25 years of experience. If you are concerned about diabetic retinopathy or any other eye condition, you can book a consultation with Mrs Mann via her Top Doctors Profile.



