Epiretinal membrane demystified: key facts for patients
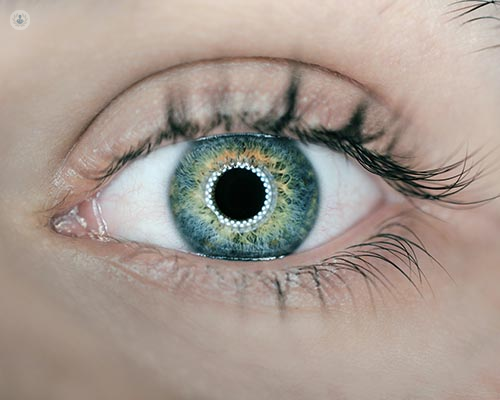
Written in association with:Epiretinal membrane (ERM), also known as macular pucker, is a condition that affects the eye's retina, particularly the macula—the central part of the retina responsible for sharp, detailed vision. Renowned consultant ophthalmic surgeon Mr Richard Haynes aims to provide an overview of ERM, its causes, symptoms, and treatment options to help patients understand this condition better.
What is epiretinal membrane?
The retina is a thin layer of tissue lining the back of the eye, and it is crucial for vision. An epiretinal membrane is a thin, fibrous layer that forms on the surface of the retina. Imagine a thin piece of cellophane or cling film lying over the retina, distorting its smooth surface. This distortion can cause visual disturbances.
What are the principal causes of epiretinal membrane?
The development of an epiretinal membrane is often related to age. As we age, the vitreous—a gel-like substance that fills the eye—can shrink and pull away from the retina. This process, known as posterior vitreous detachment (PVD), can lead to the formation of an ERM. Other causes include:
- Eye trauma: Injury to the eye can initiate the formation of an ERM.
- Inflammation: Conditions such as uveitis, an inflammation of the middle layer of the eye, can lead to ERM.
- Retinal tears or detachments: These conditions can prompt the formation of scar tissue, leading to an ERM.
- Diabetes: Diabetic retinopathy, a complication of diabetes, can also be associated with ERM.
- For no apparent reason, many ERMs develop for no apparent reason at all (probably just related to changes in within the vitreous gel collagen structure over time).
What are the main symptoms of epiretinal membrane?
Symptoms of ERM can vary depending on the severity of the condition. Some individuals may experience minimal or no symptoms, while others may notice significant changes in their vision. Common symptoms include:
- Blurred vision: The most common symptom is a gradual blurring of central vision.
- Distorted vision: Straight lines may appear wavy or bent, a phenomenon known as metamorphopsia.
- Double vision: In some cases, ERM can cause double vision .
- Difficulty reading: Fine details become harder to discern, making reading challenging.
How is epiretinal membrane diagnosed?
A comprehensive eye examination by an ophthalmologist is essential for diagnosing ERM. Diagnostic tools include:
- Optical coherence tomography (OCT): This imaging test provides detailed cross-sectional images of the retina, allowing the ophthalmologist to see the thickness and extent of the membrane.
- Fluorescein angiography: A dye is injected into the bloodstream, and images of the retina are taken to highlight blood flow and identify any abnormalities.
What are my treatment options?
Not all cases of ERM require treatment. If the symptoms are mild and not significantly affecting vision, observation and regular monitoring may be sufficient. However, if vision is notably impaired, surgical intervention might be necessary.
A vitrectomy is the most common surgical procedure to treat ERM. It involves removing the vitreous gel from the eye and peeling away the membrane from the retina's surface. This surgery is generally performed under local anaesthesia.
Post-surgery expectations
Post-operative recovery varies among individuals. Some patients may experience an improvement in vision within weeks, while for others, it may take several months. It's important to follow the ophthalmologist's instructions during the recovery period to ensure the best possible outcome.
Understanding epiretinal membrane is crucial for managing the condition effectively. If you experience any changes in your vision, it is important to seek professional advice promptly. Early diagnosis and appropriate treatment can help preserve and improve your vision.
If you would like to learn more about epiretinal membrane, book a consultation with Mr Haynes via his Top Doctors profile today.


