How pregnancy can affect the pelvic floor
Written in association with:The pelvic floor is an important group of muscles and connective tissues that support the organs within. When weakened, incontinence, among other problems, can result. Ms Charlotte Chaliha, an expert obstetrician and gynaecologist, discusses the importance of the pelvic floor and why some women experience problems with it.
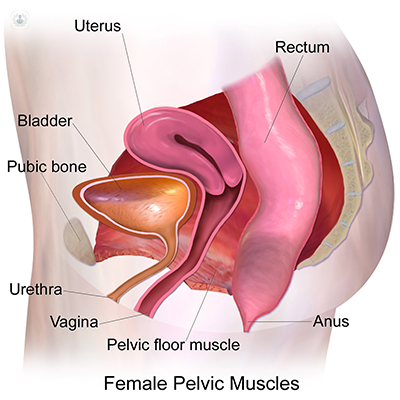
What is the pelvic floor?
The pelvic floor organs sit supported within the pelvis by the muscles of the pelvic floor. These are called the levator ani and provide support, alongside connective tissue supports. Changes in the structure of the levator muscle (the basin-like muscle that is the pelvic floor) can be seen after vaginal delivery birthing. These are similar to the changes seen in women with pelvic floor prolapse and stress incontinence of urine. Vaginal delivery results in over-distension of the levator muscles as well as avulsion of the portion of the muscle (puborectalis) from its strong bony insertion point. In approximately 25% of women, this over-distension is irreversible.
What does my pelvic floor do?
The female pelvic floor muscles support the pelvic organs and maintain continence. They are important for good sexual function, as well as good control of urination and defecation.
How does pregnancy affect the pelvic floor?
One in every three women will have incontinence during her lifetime and of these up to 65% will recall that it began either during pregnancy or after childbirth. Clinical and epidemiological studies strongly indicate that women who undergo vaginal delivery are at higher risk of subsequent incontinence than women who have never delivered or and those who undergo a caesarean section. This is most likely related to the detrimental impact of vaginal delivery on the pelvic floor. Furthermore, it seems that the first vaginal delivery is the time when women sustain most damage, comparative to subsequent births via vaginal delivery.
Supporting these findings are several studies showing a relationship between vaginal delivery and mechanical and neurological damage to the pelvic floor which are related to the development of urinary or anal incontinence, or both. There may also be women at an increased predisposition to pelvic floor trauma, incontinence and prolapse, due to an inherent weakness of collagen within the pelvic floor tissues.
In addition to this, vaginal childbirth is associated with a high risk of perineal trauma (tears in the perineum and vagina) which occur in around 85% of women.
How can I strengthen my pelvic floor?
The following are recommended for strengthening the pelvic floor:
- Pelvic floor physiotherapy with a specialist
- Avoidance of chronic straining (such as constipation) and heavy lifting
- Avoidance of excessive weight gain
What advice can you give to new mums on managing their pelvic floor?
Pelvic floor physiotherapy with a specialist physiotherapist, ideally to start in the antenatal period and to continue after pregnancy. For a few mothers, a discussion on avoidance of vaginal delivery if the baby is very large will need to be had, as there is a risk of significant trauma to the pelvic floor. In addition, mothers who have had previous damage to their anal sphincters (so-called third and fourth-degree tears) may need to be counselled carefully on their mode of delivery in future pregnancies. For some, a detailed assessment of the anal sphincter is advisable before the next pregnancy.
If you are concerned about your pelvic floor, or your next delivery, make an appointment with an expert to discuss your options.


