How to heal a fracture
Written in association with:If you, or someone you know, has cracked or broken a bone, it would be clinically referred to as a fracture. The human body has methods to heal itself, but with the assistance of an orthopaedic surgeon, the likelihood that the bone will heal fully in the correct position and with fully restored mobility is much, much higher. Mr Rohit Madhav, a consultant orthopaedic surgeon, explains how a fracture is healed.
What exactly is a bone fracture?
A fracture, in any context, is when a hard object or material is cracked, shattered or broken. For the human body, a fracture is a consequence of direct or indirect physical trauma, repetitive but less severe injuries or a condition that weakens the bones, such as osteoporosis.
- Traumatic injury: Physical trauma is caused by a hard impact. This can be due to events such as a serious fall, a car accident or sports injury.
- Medical conditions: Bones become thinner and less durable as people age, but people with osteoporosis have even more brittle bones. As a result, the bones can break much more easily than someone younger or an elderly person without osteoporosis. This is because the bones can’t cope with as much physical stress.
Types of fractures
While fractures are generally referred to as cracked or broken, there are specific types that a medical specialist can identify. The following are the most common types of fractures.
- Simple fractures: If a patient arrives with a fracture but the bones are in a stable position and barely out of place, it’s referred to as simple. This is relatively easier to treat than other types. Think of the two broken ends of bone still being near where they were before the break.
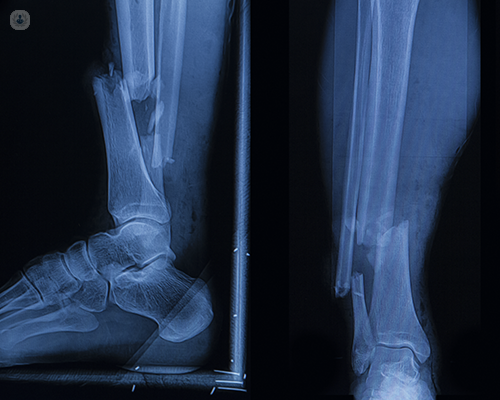
- Unstable fractures: These fractures are when a bone is not in a stable position and out of place. Think of when the two broken ends of a bone aren’t meeting near where they should.
- Open (compound) fractures: These are severe and can be distressing. Open fractures have pierced the skin and created an open wound. Because the skin has been pierced by the bone, leading to an open wound, infection is a possibility and the injury must be dealt with immediately to avoid this. The bone might be visible in the wound, but not always.
- Greenstick fractures: Children’s bones are softer than adult bones. Greenstick fractures are specific to children, most commonly in those under 10 years old. Rather than fully breaking, the bone bends on one side but not the other.
The body’s healing response
When a bone is cracked or broken, the body begins self-healing with a few key responses. These are:
- a blood clot.
- a callus (a growth of tissue that stabilises the fracture by forming around the broken ends of the bone).
- fibrous tissue (hard scar tissue that forms around injuries to reattach torn muscle).
Medical treatment
First and foremost, when treating a fracture in the early stages, the goal is to manage bleeding and prevent as much bone as possible from dying (ischaemia). In the particular case of open fractures, a specialist will want to remove foreign bodies and tissue before an infection has the chance to occur.
The next step involves setting the bone back into its natural position and this is clinically referred to as “reducing the fracture”. The objective of any orthopaedic specialist is to restore the function and mobility of the injured bones to how they were before the injury. In order to achieve this, your specialist will choose a non-operative treatment or surgery, depending on the injury.
Non-operative methods
Once the condition is stable, a non-operative method may be chosen.
- An orthopaedic cast or splint: If a fractured bone is out of place, shortened or bent, a patient may be offered a cast or splint. These are formed around the limb and stop the limb from moving so that the bone can heal.
- Traction method: When a bone is fractured or dislocated and a cast isn’t suitable, the next option is one of the two traction methods: skin traction or skeletal traction. Skin traction involves using tapes that attach to the limb and skeletal traction involves inserting pins into the bone.
Surgical methods
Surgery is performed for serious fractures that aren’t treatable with a cast, splint or traction.
- ORIF (open reduction internal fixation): “Open reduction” refers to the process of repositioning the bones and “internal fixation” refers to the follow-up stage of holding the bones together. The newly repositioned bones can be held in place with clinical tools such as kirschner wires, plates and screws, and intramedullary nails.
- External fixation: This is an external metal device with screws that reach from the device into the bone. Screws are placed above and below the fracture to facilitate the preservation of bone length and to keep it realigned without the need for a cast.
External fixation may be used for:
- open fractures with soft-tissue involved in the break.
- injuries involving burns and soft tissue.
- pelvic fractures.
- a comminuted fracture (when the bone is broken in more than two places) and unstable fractures.
- limb-lengthening procedures.
- fractures with infection.
Rehabilitation
The time needed for a fracture to heal depends on the severity of the crack or break: it can take weeks or months. Even after medical treatment is complete, you should still be aware that the bone may still be weak. By monitoring your activity level, you can give the bone a chance to become stronger and cope with stress. In some cases, healing can be enhanced by the use of ultrasonic bone stimulators placed externally over the broken bone such as the Exogen® system.
With a rehabilitation program, you’ll be assisted in gradually increasing your activity level until the healing process is fully complete.
Visit Mr Rohit Madhav’s profile to get in touch and have your orthopaedic doubts and pains resolved.


