Liver disease: one of the UK’s biggest killers
Written in association with:Liver disease is in the top five causes of premature death in the United Kingdom. Over the past decade, there has been a 20% increase in the number of cases of liver disease, which is quite dramatic, but how much do you know about liver disease? Professor Kevin Peter Moore has nearly 25 years of experience as a consultant hepatologist (liver specialist), including 20 years of liver transplantation, as well as general hepatology. Hence, he has experience in treating all forms of liver disease, and here he gives us a thorough overview.

What is liver disease?
Liver disease takes on various forms:
- Fatty liver disease.
- Repetitive liver injury from too much alcohol (whether it be beer, wine or spirits).
- Chronic hepatitis caused by viral infections (hepatitis B and hepatitis C).
- Autoimmune liver disease (when the body attacks the liver).
- An inherited disease such as haemochromatosis or Wilson’s disease.
- Diseases involving inflammation of the bile ducts or ductules, such as primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC), or an inherited condition of bile acid transport.
The primary consequence of each of these conditions is chronic inflammation of the liver. Chronic inflammation leads to scarring or fibrosis of the liver and premature death of liver cells. Although the liver has the capacity to regenerate, it cannot do so whilst there is ongoing inflammation. Thus, if you treat chronic viral hepatitis early enough to prevent cirrhosis, the liver can recover, or if you stop drinking alcohol before you have caused irreversible liver scarring and cirrhosis, the liver can also recover over time.
Hence, the most important thing about liver disease is to prevent chronic liver injury degenerating into cirrhosis, which over time leads to liver cancer and/or liver failure.
Why is liver disease on the rise in the UK?
The main drivers for the increase in liver disease are alcohol and fatty liver disease.
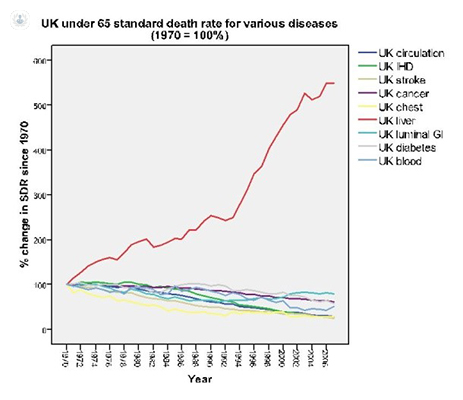
Deaths from liver disease in the population aged over 60 years have been increasing dramatically over the last 30-40 years (see the red line on the chart below), compared to their baseline in 1970. All other causes of death are decreasing except liver disease.
Fatty liver disease is becoming a more important cause of cirrhosis with the obesity epidemic and increases in type 2 diabetes in the general population are both risk factors for cirrhosis.
How can liver disease be diagnosed?
Liver disease is diagnosed or suspected when there are abnormal liver function tests or abnormalities found on a liver ultrasound scan, CT liver scan or MRI imaging of the liver. These scans may also pick up liver cysts (usually harmless), liver haemangioma (also harmless), focal nodular hyperplasia (harmless) or gall bladder polyps (also frequently harmless but they may need monitoring).
Why should I see a hepatologist (liver specialist) for treatment?
Many patients with liver disease are diagnosed and treated by a general gastroenterologist, although most will have an interest in liver disease. However, in my view, most patients should see a hepatologist who specialises in liver disease and ideally has extensive experience.
Together with good treatment, and a change in lifestyle for some, the outcome or prognosis for many forms of liver disease can be improved dramatically.
What is the best treatment for liver disease?
There is no such thing as the best treatment for liver disease as it depends on the cause. The role of your hepatologist is to diagnose the cause of your liver disease, exclude all other treatable causes of liver disease, and offer you the best advice and treatment for your liver condition.
If you are concerned about your liver health and associated lifestyle habits, book an appointment with Professor Kevin Peter Moore to have a liver health check.


