Mastectomy: can I have breast reconstruction?
Written in association with:The decision to have a breast reconstruction is a personal one that should be taken carefully, but if you decide this surgery is for you, there are several aspects you might need to take into account. In this article, leading consultant oncoplastic breast surgeon Mr Jaroslaw Krupa, provides a comprehensive overview of the procedure, explaining if it’s possible to have a mastectomy and breast reconstruction at the same time, if breast reconstruction can lead to a return of cancer, and what some of the results that patients can expect are.
What are my breast reconstruction options?
Women who have had mastectomy or lumpectomy may choose to have breast reconstruction to rebuild the shape of the lost breast and restore breast contour. Breast reconstruction can also be performed at the same time as mastectomy or lumpectomy in a procedure called immediate reconstruction. In fact, the National Institute of Clinical Excellence (NICE) recommends that immediate breast construction should be offered to all patients facing a mastectomy if this is clinically appropriate.
There are several other options available for breast reconstruction, which will be detailed now below:
- An autologous tissue reconstruction involves transferring a patient's own tissue from a different part of the body to the breast area. This operation most commonly uses muscle from the back (latissimus dorsi) or the abdominal tissue (DIEP or TRAM flap).
- The most popular type of breast reconstruction in the UK and worldwide involves the use of silicone implants. There is an extensive range of implants available, suitable for various breast shapes and sizes. Additional use of biological or synthetic mesh can also improve cosmetic outcomes after surgery. This type of procedure does not result in any additional scarring outside the breast area, which is an important consideration.
- Breast cancer reconstruction can be quite complex for some patients, as is the experience of being diagnosed with breast cancer. For patients who find it difficult to make a decision about breast reconstruction, delayed reconstruction (performed after breast cancer surgery) may be the preferable option. It allows time to concentrate on cancer treatment first and then consider reconstruction at a later stage.
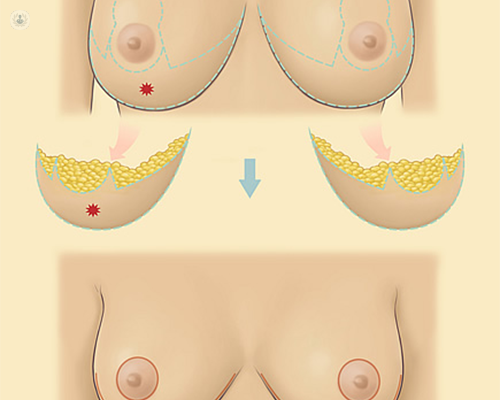
- There are some technical considerations which are important and can be very relevant for individual patients. For example, modern reconstructive techniques often allow preservation of the skin covering the breast when performing mastectomy. This procedure, called skin-sparing or nipple-sparing mastectomy, can significantly enhance the outcome of breast reconstruction. If the patient opts for delayed reconstruction, then the majority of skin is removed during mastectomy and needs to be restored at la ater stage.
- Delayed reconstruction may also be more appropriate if the cancerous tumour invades the skin or the disease is more advanced at the time of diagnosis. From the perspective of cancer treatment, it is more advisable to remove the skin rather than trying to preserve it, which may result in incomplete excision of cancer. In these scenarios, delayed reconstruction could offer better results for the patient.
- Finally, there are some instances in which breast cancer patients will require additional treatments like chemotherapy or radiation therapy after surgery. In these situations, radiation can have a detrimental effect on reconstruction and patients may find themselves in a situation where breast reconstruction initially looks very good after surgery and then may deteriorate after radiotherapy.
What type of breast reconstruction is best for me?
When reconstruction is considered, there are several issues that a breast surgeon will take into account to determine which type of breast reconstruction is best for each patient.
The first and foremost is the oncological aspect of treatment, which should always take priority in any decision-making process. It’s not the cosmetic outcome, but the treatment of the cancer which is more important, and all surgical strategies are built around that.
The second one involves the patient’s general health and other medical conditions, which can limit some reconstructive options. Patients who opt for abdominal flap reconstruction (DIEP flap) may not be good candidates, for example, if they have previously undergone extensive abdominal surgery, and if they have scarring in the abdomen. These are lengthy operations that require microsurgical procedures as well, so breast reconstruction will not be suitable for patients with significant comorbidities.
Another consideration is breast shape, size, and symmetry. It can be sometimes challenging to reconstruct a breast with the same size or shape as a healthy breast. Some patients have to consider either increasing or decreasing the volume of the breast through a procedure called symmetrisation surgery. These operations are performed on a healthy breast to improve overall symmetry. Examples include a breast uplift, augmentation, or reduction.
A patient’s expectations regarding reconstruction are also taken into account by a breast surgeon. The expected result of breast reconstruction is one of the most important considerations and requires detailed discussion and multiple consultations. The breast surgeon will try to understand a patient’s expectations and try to communicate possible options from the surgical point of view. Although breast reconstruction can often achieve excellent results, this procedure is not a cosmetic operation done purely for aesthetic reasons.
Improving body image and restoring the breast after cancer treatment can have tremendous psychological benefit for the patient, but a reconstructed breast isn’t as good as a natural breast. It will not look or feel the same and the patients often experience a so called “adjustment period” before making a full recovery from reconstruction.
The safety of breast reconstruction has also been documented in several clinical studies, which show that breast reconstruction does not have a detrimental effect on cancer outcomes, including the risk of cancer recurrence and overall cancer survival.
Breast reconstruction support groups can be a very valuable source of information on various types of procedures and possible outcomes. All patients facing a decision about reconstruction are also supported by specialist breast care nurses and provided with additional written information.
Mr Jaroslaw Krupa is a highly experienced consultant oncoplastic breast surgeon based in Leicester and Nottingham, who specialises in breast cancer, breast reduction, breast augmentation and mastopexy. If you’re thinking about breast reconstruction and wish to consider your options, don’t hesitate to visit Mr Krupa’s Top Doctors profile today.


