Retinal detachment: Early detection and treatment
Written by:Retinal detachment is a serious and vision-threatening eye condition that requires immediate medical attention.
Here, Mr Serafeim Antonakis, renowned consultant ophthalmologist and vitreoretinal surgeon, provides a comprehensive overview of retinal detachment, including its signs and symptoms, causes, and treatment options.
What is retinal detachment?
Retinal detachment occurs when the retina, a thin layer of tissue at the back of the eye responsible for sensing light and sending visual signals to the brain, separates from its normal position. This separation can result in the retina being deprived of essential oxygen and nutrients, leading to potential vision loss if not treated promptly.
What are the signs of retinal detachment?
The signs of retinal detachment can occur suddenly and without warning. It’s important to recognise them early in order to seek timely medical intervention.
Common symptoms include:
- the sudden appearance of floaters
- brief flashes of light, often in the peripheral vision
- a dark shadow or curtain that starts to obscure vision from one side
- a noticeable and sudden decrease in visual clarity
What causes retinal detachment?
Retinal detachment can be triggered by various factors, often related to changes or damage within the eye. Here are the primary causes:
- Ageing: As we age, the vitreous gel inside the eye can shrink and pull away from the retina. This process, known as posterior vitreous detachment (PVD), can create a tear in the retina. Fluid from the vitreous gel can then seep through the tear, causing the retina to detach.
- Eye injuries: Trauma to the eye can lead to retinal detachment. Blunt force or penetrating injuries can damage the retinal tissue directly or cause it to detach from the underlying layers.
- Diabetic retinopathy: People who have diabetes are at risk of developing diabetic retinopathy, a condition where high blood sugar levels damage the blood vessels in the retina. This damage can lead to the growth of abnormal blood vessels, which can pull on the retina and cause detachment.
- Severe near-sightedness (myopia): People who have severe myopia often have elongated eyeballs, which can increase the strain on the retina and make it more susceptible to tears and detachment. The thinner retinas in myopic eyes are more prone to degenerative changes.
How is retinal detachment detected and diagnosed?
Early detection of retinal detachment is vital for preserving vision.
An ophthalmologist will conduct a thorough eye examination, which includes:
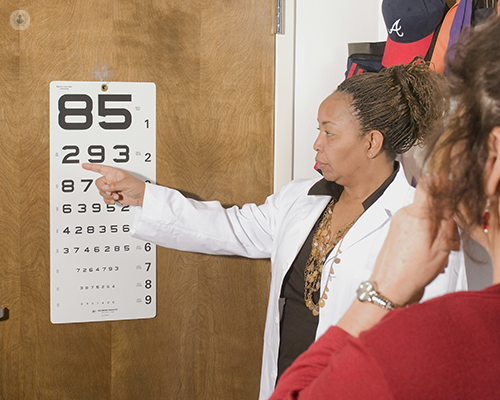
- A visual acuity test: The test measures how well an individual can see at various distances.
- A dilated eye exam: Special drops are used to widen the pupils, allowing the ophthalmologist to examine the retina more thoroughly.
- An ophthalmoscopy: A tool called an ophthalmoscope is used to look at the back of the eye, including the retina.
To get a detailed view of the retina, the ophthalmologist may use several imaging tests such as:
- Ultrasound: An ultrasound is especially useful if there is bleeding in the eye, making it difficult to see the retina directly.
- Optical coherence tomography (OCT): An OCT scan provides detailed cross-sectional images of the retina.
These diagnostic tools help in confirming the presence of retinal detachment and assessing its severity.
What treatment options are available for retinal detachment?
The treatment for retinal detachment depends on the severity and type of detachment. Here are the primary treatment options:
- Photocoagulation (laser surgery): Laser photocoagulation involves using a laser to create small burns around the retinal tear, causing scarring that seals the retina to the underlying tissue. This procedure is often performed in the ophthalmologist’s office and can prevent detachment if caught early.
- Cryopexy: Cryopexy uses extreme cold to create a scar that helps reattach the retina. The procedure is similar to laser surgery in terms of its purpose and is also performed in a clinical setting.
- Pneumatic retinopexy: In this procedure, a gas bubble is injected into the vitreous cavity inside the eye. The bubble presses against the detached retina, helping it to reattach. This procedure is often combined with laser or freezing treatment to seal the tear.
- Scleral buckling: Scleral buckling involves placing a silicone band around the eye to gently push the wall of the eye against the detached retina. This method can be used for more severe detachments and often requires surgery in a hospital setting.
- Vitrectomy: Vitrectomy is a surgical procedure where the vitreous gel is removed and replaced with a gas bubble, silicone oil, or saline solution. This method is typically used for more complex cases of retinal detachment.
Each treatment option has its own risks and benefits, which should be discussed with the ophthalmologist to determine the best approach for the individual patient.
Is retinal detachment preventable?
While it is not always possible to prevent retinal detachment, certain measures can reduce the risk, including:
- Attending regular eye examinations to help detect early changes in the retina
- Managing chronic conditions such as diabetes
- Wearing protective eyewear during activities that could cause eye injuries
- Being aware of the symptoms of retinal detachment
If you would like to schedule an appointment with Mr Serafeim Antonakis, head on over to his Top Doctors profile today.


