The role of radiotherapy for prostate cancer
Written in association with:Radiotherapy is a highly targeted and specialised treatment that can be used to treat the different stages of prostate cancer, improving survival.
Here to provide an expert insight into radiotherapy for prostate cancer is Dr Albert Edwards, renowned consultant clinical oncologist based in Canterbury and Maidstone.
How important is radiotherapy in terms of treating prostate cancer?
Radiotherapy is a very important treatment across the whole range of prostate cancer.
It is one of the important curative treatments for localised prostate cancer; it has a very important role in treating more advanced prostate cancer; and it has a role in palliative, incurable prostate cancer.
In fact, it has been shown in the STAMPEDE trial that delivering radiotherapy to the prostate improves survival in certain patients whose cancer has spread.
How effective is radiotherapy when it comes to treating prostate cancer?
For potentially curable prostate cancer, radiotherapy and surgery are as effective as each other, but they have very different side effect profiles. Thus, it is important to consider the short-term and the long-term potential side effects of both treatments, in order to make an informed decision.
For advanced and incurable prostate cancer, radiotherapy (such as palliative radiotherapy) to the prostate or to the areas of cancer deposits is very important to relieve symptoms and improve quality of life.
What exactly does radiotherapy involve and consist of?
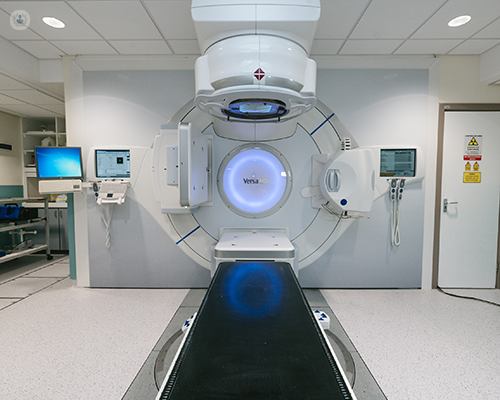
When it comes to prostate cancer, external beam radiotherapy is the standard type of radiotherapy used.
External beam radiotherapy uses high-energy X-ray beams to damage cancer cells. By building up this damage in multiple treatment sessions, we hope to kill the cancer, cure the patient, and preserve the tissues that the cancer was standing in (called organ preservation) as opposed to actually cutting them out.
The X-ray beams that are used are invisible, just like the low-energy X-rays that are used for taking CT and X-ray scans. However, this means that we must be absolutely sure where the high-energy X-rays are going during each treatment session to not miss the target.
The modern treatment for curative radiotherapy for prostate cancer is called image-guided intensity-modulated radiotherapy (IG-IMRT). This is a type of targeted external beam radiotherapy that uses real-time imaging scans to adapt the X-ray beams to the tumour.
With IG-IMRT, we will check that the prostate is where it is believed to be before each treatment session is delivered.
This will be done either:
- With a quick scan to latch onto seeds that have been implanted into the prostate to ensure that it has not moved.
- With a combined CT scan to check the position of the prostate.
If the prostate has moved, we must then ensure that the radiotherapy dose always covers the entire tumour during each treatment session.
Are prostate cancer survival rates increased thanks to radiotherapy treatment?
More than 50,000 people are diagnosed with prostate cancer each year in the UK. Many will have radiotherapy at some point during their treatment. This is because radiotherapy can be an extremely important curative treatment in selected patients and an important contributor to the survival rates of prostate cancer.
As of now, there are ongoing clinical trials all around the world looking to improve radiotherapy treatment and increase the cure rates even further.
How long would an average patient have to undergo radiotherapy treatment?
The length of radiotherapy treatment entirely depends on the nature of the tumour and on how far it has spread.
Curable prostate cancer tends to be divided into risk categories: low, intermediate, and high risk.
Generally, low risk patients are offered active surveillance. Hopefully, these patients can remain on surveillance for many years before they eventually need to have curative treatment with radiation, surgery, or brachytherapy.
Intermediate risk patients are typically offered six months of hormone treatment and then four weeks of daily radiotherapy to the prostate during the fourth month.
High risk patients are usually offered a longer course of radiotherapy and a longer course of hormone treatment. These patients will receive two to three years of hormone treatment and their radiotherapy may last four weeks (or eight weeks Monday to Friday, in some cases).
Treatment is tailored according to the patient's prostate cancer and their individual situation.
Can radiotherapy help cure prostate cancer?
Yes, radiotherapy is an important part in treating curable prostate cancer.
As well as this, radiotherapy can also contribute to patients who have undergone a prostatectomy (prostate removal). This is because patients who have had their prostate removed can experience prostate cancer recurrence. It has been shown in three large, randomised trials that delivering radiation to the area where the prostate was removed is the best treatment option for these patients.
Dr Albert Edwards is a highly skilled consultant clinical oncologist with more than 20 years of experience.
If you require radiotherapy for prostate cancer and wish to consult your options with an expert, do not hesitate to book an appointment with Dr Edwards today via his Top Doctors profile.


