Treatment of hip arthritis with total hip replacement
Written in association with:Hip arthritis, particularly osteoarthritis, is a common condition that affects many individuals, especially as they age. This degenerative joint disease can cause significant pain, stiffness and mobility issues, ultimately impacting a person’s quality of life. When conservative treatments such as medication, physical therapy and lifestyle modifications fail to provide relief, a total hip replacement (THR) may be recommended as an effective solution. Here to tell us all about it, is leading orthopaedic surgeon Mr Rajpal Nandra.

What is a total hip replacement?
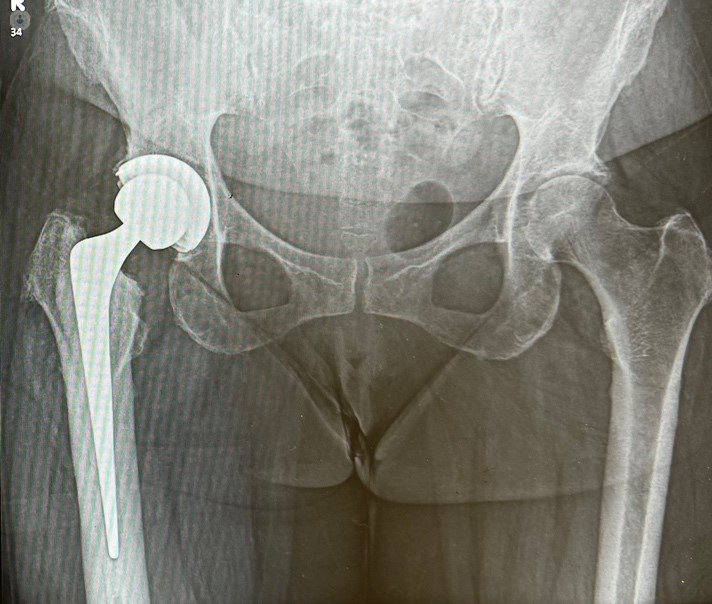
Total hip replacement, also known as hip arthroplasty, is a surgical procedure that involves replacing the damaged hip joint with a prosthetic implant. The procedure is designed to relieve pain, restore function and improve the overall quality of life for patients suffering from severe hip arthritis.
During the surgery, the orthopaedic surgeon removes the damaged cartilage and bone from the hip joint. This typically involves:
- Femoral component: The top of the thigh bone (femur) is replaced with a metal stem that is inserted into the femur, with a metal or ceramic ball attached to the top.
- Acetabular component: The socket part of the hip joint (acetabulum) is resurfaced. A metal cup with a plastic or ceramic liner is placed into the socket.
These components work together to replicate the natural movement of the hip joint, allowing for a smoother, pain-free range of motion.
When is total hip replacement necessary?
Total hip replacement is usually considered when hip arthritis causes persistent, debilitating pain and interferes with daily activities such as walking, climbing stairs or even resting. The decision to undergo THR is based on several factors:
- Severity of symptoms: When pain, stiffness and reduced mobility severely limit your ability to perform daily tasks, and other treatments have been ineffective.
- Impact on quality of life: When hip arthritis significantly affects your quality of life, causing emotional distress or preventing you from enjoying activities you once loved.
- Response to non-surgical treatments: If medications, physical therapy or lifestyle changes have not provided sufficient relief, surgery may be the next step.
Recovery and outcomes
Recovery from total hip replacement surgery spans six weeks. The surgical wound takes two weeks to heal. The absorbable suture just under the skin does not need to be removed. You will walk and climb stairs the day after surgery but need crutches for up to four weeks. Some patients require physiotherapy to maximise strength, flexibility and mobility. We routinely prescribe blood thinning tablets for 35 days after surgery to reduce the risk of deep vein thrombosis.
The outcomes of THR are generally very positive, with most patients experiencing:
- Pain relief: The primary benefit of THR is the significant reduction or elimination of hip pain, allowing patients to resume normal activities.
- Improved mobility: Many patients regain the ability to walk, climb stairs, and participate in low-impact activities that were previously too painful, including recreational sports.
- Enhanced quality of life: With reduced pain and improved mobility, patients often experience an overall improvement in their quality of life.
What are the risks and considerations associated with THR?
As with any surgery, there are risks associated with total hip replacement. These may include infection, blood clots, dislocation of the implant, or wear and tear on the prosthetic components over time. However, advances in surgical techniques and implant materials have greatly improved the safety and durability of the procedure.
Total hip replacement is a highly effective treatment option for patients with severe hip arthritis. It can provide long-term relief from pain, improve mobility, and enhance the quality of life. If you are suffering from hip arthritis and are considering surgery, consult with an orthopaedic surgeon to determine if total hip replacement is right for you.
Do you have hip arthritis and require total hip replacement? Arrange a consultation with Mr Nandra via his Top Doctors profile.


