What are the different types of ultrasound scans in pregnancy?
Written in association with:Did you know there’s more than one type of ultrasound scan in pregnancy? They are undertaken depending on the stage of the pregnancy, and also for various reasons such as calculating the chances of the pregnancy being affected with Down’s syndrome and risk of going into preterm labour, and many more.
Here to explain these different ultrasound scans is highly-experienced consultant in maternal-fetal medicine (MFM) and obstetrics, Dr Srividhya Sankaran.

Types of scans during pregnancy
- Early pregnancy or dating scan (8-11 weeks)
- Nuchal Translucency scan (11-14 weeks)
- Early Anomaly scan (14-18 weeks)
- Fetal Anomaly scan (19-23 weeks)
- Growth scan or Fetal Wellbeing scan (24-42 weeks)
- Recommended at 36 weeks
- Optional - four weekly, more frequently in some conditions
Early pregnancy/dating scan (8 - 11 weeks)
This scan is done to confirm a pregnancy and to determine an estimated pregnancy due date (EDD). A foetal heart rate is detected during this scan. Most parents opt for this scan for reassurance. Also knowing this date by scan is essential prior to the blood test called as non-invasive prenatal test (NIPT) to calculate the chances of pregnancy being affected with Down’s syndrome. This scan is done on your tummy. Occasionally an internal scan may be required to get more information and a clearer picture.
Nuchal Translucency scan (11-14 weeks)

This is usually performed abdominally and occasionally an additional internal scan may be needed.
This scan is done to:
- Confirm that the baby’s heart is present;
- To estimate the duration of pregnancy more accurately. This may not be necessary in pregnancies conceived by IVF, where the dates calculated from the transfer of embryo is more accurate;
- To measure the length of baby;
- To diagnose whether more than one baby is present and to assess whether there is sharing of placenta, which will need close monitoring in pregnancy;
- To assess the structure of the foetus including measurement of fluid in the back of baby’s neck;
- To see if there is a low or high chance for the baby to be affected with common chromosomal problems such as Down’s Syndrome, Edward’s Syndrome and Patau syndrome;
- If any abnormality is found on initial scan, further detailed assessment and counselling regarding further options will be provided at the same assessment by myself.
Blood tests to screen for Down’s syndrome – for biochemical as well as free-foetal DNA testing (otherwise known as Non-invasive Prenatal testing or NIPT) may also be offered on request.
Early anomaly scan (14 - 18 weeks)

Please see below. It’s the same as 19-22 weeks, but some structures of the baby may be too small or in the developing stages and it may not be possible to confirm the normality. Usually this is offered if there are known risk factors for abnormalities such as spina bifida or if parents are keen to know the sex of the baby earlier. These scans may be done earlier, however some of the structures might not be visualised and hence, a repeat scan at 19-22 weeks is needed to confirm.
Foetal anomaly scan (18 - 24 weeks)

This scan is done usually at 19-22 weeks. It’s a systematic check from head to toe of the baby to see if the structures appear normal as expected for this age. This is the scan, where most of the abnormalities get picked up, when present.
If any abnormalities are present, the foetal medicine experts will look at more details to obtain information. Our consultants are also experts in assessing the normality of foetal brain and heart. With this information, our foetal medicine consultants provide you with explanation of the findings, implication, further referral to specialists such as foetal cardiologists if necessary and counselling about further options.
During this scan, the position of the placenta and blood flow through placenta will also be assessed. This information will aid further management plans in pregnancy.
Additionally, the risk of going into preterm labour can be predicted by measuring the length of cervix by an internal scan.
Growth scan 24 weeks onwards

- Growth and well-being of the baby is monitored by these scans after 24 weeks.
- Specific measurements of head, abdomen and thigh are done to arrive at an estimated foetal weight centile of the baby.
- Amniotic fluid volume around the baby is measured.
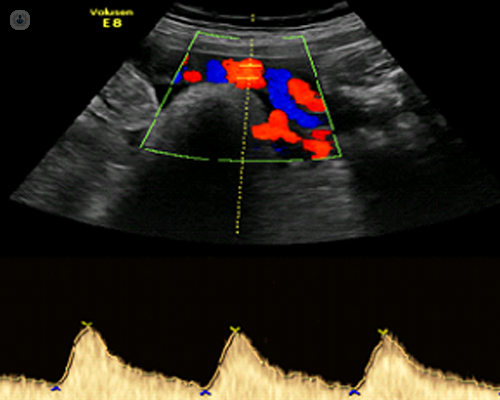
- Blood flow through umbilical cord and baby’s blood vessels are checked. (Baby Doppler scans)
The way baby lies in mother’s womb nearer the time of birth is useful to plan delivery. Occasionally, an abnormality which was not seen in the baby before may be picked up on these scans.
If any abnormalities are suspected, I will explain them to you, arrange appropriate follow-up and will make birth plans based on the assessment.
If no problems are suspected, these scans may be repeated every four weeks to monitor the growth. Depending on the findings, a follow-up may be offered earlier than four weeks.
3D scans: Available for every scan
During all the above scans, a 3D scan (of the baby) can also be performed. The clarity of pictures is dependent on the position of the baby, placenta, umbilical cord, amount of amniotic fluid and thickness of mother’s tissue.
Blood tests that may be advised along with scan, for screening for Down’s syndrome and similar chromosomal abnormalities
- Biochemical testing
First trimester Combined Screening Test: This includes blood test for biochemical markers, along with nuchal translucency scan;
Quadruple test: This includes blood test for biochemical markers, along with anomaly scan (14-20 weeks).
- Fetal DNA testing (which is a superior test to biochemical tests)
Non-Invasive Prenatal Testing (NIPT), Harmony test. From 10 weeks onwards. A scan is essential before this test is done.
If you’re looking for London-based MFM and obstetric care, arrange a consultation with Dr Sankaran via her Top Doctors profile.


