What's the best treatment for osteoporosis?
Written in association with:The best treatment for osteoporosis typically involves a combination of lifestyle changes, medications, and supplements aimed at strengthening bones, preventing fractures, and slowing down bone loss. A condition where bones become weak and brittle, it often affects older adults, particularly postmenopausal women. A personalised treatment plan is essential, as the best approach can vary depending on the severity of the condition, age, and overall health of the individual. Here to tell us all about it, is leading specialist in integrative medicine Dr Federica Boecklin.

What lifestyle changes can I make to prevent osteoporosis?
- Diet: Diet and lifestyle play a crucial role in the prevention and management of osteoporosis, and the good news is that simple changes can significantly reduce the risk of bone loss. A high-quality, nutrient-rich diet, rather than focusing on individual supplements like calcium, zinc, or protein, can reduce the risk of osteoporosis by as much as 30 to 40 per cent. The key is an overall healthy diet, particularly one that includes plenty of vegetables, limits ultra-processed foods, and emphasises plant-based foods, which support bone health. This is especially important during perimenopause and menopause, when women experience hormonal changes that can increase their risk of osteoporosis.
- Exercise: Exercise is another critical factor in maintaining strong bones. The important distinction here is that weight-bearing exercises, which apply pressure to the bones, are the most effective for bone health. Activities like skipping, jumping, or weightlifting are particularly beneficial because they create impact or shock on the bones, stimulating bone formation and strengthening bone density. While exercises like swimming are excellent for muscle strength and cardiovascular health, they don’t provide the necessary pressure on bones to promote bone density. Incorporating weight-bearing activities into your routine to support bone health is essential.
- Avoiding smoking and excessive alcohol: Both smoking and high alcohol consumption can accelerate bone loss. Quitting smoking and moderating alcohol intake are key steps to preserving bone health.
How can you make sure you get enough calcium from food?
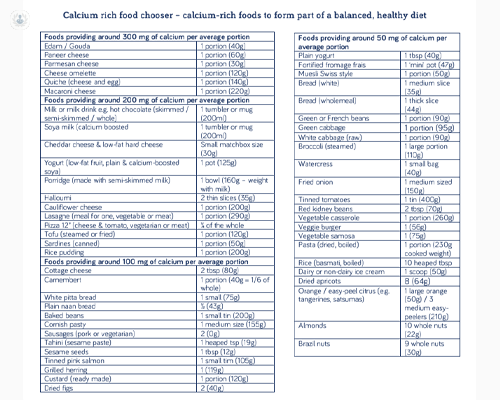
Refer to the table below to remind yourself of foods rich in calcium that should be included in your diet.
Aim for 700 to 1000 mg of calcium daily to make sure you get enough.
What are the best exercises to prevent osteoporosis?
Weight-bearing exercise with added impact or force
Everyone needs to do about 50 moderate-impacts on most days of the week. That includes you if you have osteoporosis. The impacts could be jumps, skips, jogs or hops. One jump counts as one impact. This is physical activity where you are supporting the weight of your own body, so the weight of your body pulls on your skeleton.
Include some impact if you can, which could include jogging, aerobics, tennis, dancing, or brisk walking. It's essential to do what you can manage. Build up gradually from low-impact to moderate to high-impact exercises.
Low impact
- Walking
- Brisk walking
- Marching
- Stamping
- Stair climbing
- Gentle heel drops
- Hill walking
Moderate-impact
- Highland dancing
- Jogging
- Running
- Team sports
- Racket sports
- Skipping and hopping
- Low level jumps
- Heel drops with more force
- Stamping with more force
- Nordic walking
High-impact
- Basketball
- Volleyball
- Track events
- Star jumps
- Tuck jumps
- High-level jumps
- Muscle-strengthening exercise: This is any movement where you are working against resistance. This could be a weight in your hand, a resistance band, or your body weight, such as during a press-up. If you can, increase the intensity gradually with stronger resistance bands or heavier weights.
It’s recommended to do this type of exercise with this frequency:
- on 2 to 3 days of the week – leave at least a day’s rest in between
- for 20 to 30 minutes – work on your legs, arms and spine
- gradually using bands and weights – lift the most weight you can do for 8 to 12 repetitions
Build up to 3 sets of each exercise – 1 set is 8 to 12 repetitions.
Reducing the risk of a fall
Preventing falls is another crucial component of osteoporosis treatment, as even minor falls can lead to fractures in people with brittle bones. Measures like improving home safety, using assistive devices, and strengthening balance through exercises can help reduce the risk of falls.
Exercise to keep steady
Falling over is a major cause of broken bones (especially broken hips) in people with osteoporosis, so it’s vital to do exercises that help to maintain or improve balance. Exercises like swimming, gardening, golf and Tai Chi may help you maintain muscle strength, balance, and coordination and reduce your risk of falling.
If you struggle with your balance, begin with some balance-improving exercises before increasing your activity levels in other ways. Once you’re more confident with your balance, start with simple forms of activity such as brisk walking.
In summary, the best treatment for osteoporosis involves a comprehensive approach combining medications, lifestyle modifications, and supplements to improve bone strength, prevent fractures, and slow the progression of the disease. Consulting with a healthcare professional is essential to developing an individualised plan.
Supplements
- Calcium supplements: Calcium supplementation for osteoporosis prevention has become a topic of increasing debate. While calcium was once widely recommended for bone health, recent evidence suggests that routine supplementation may not be beneficial—and could even be harmful in some cases. Studies have shown no conclusive benefit in reducing fracture risk from calcium supplements, and there are concerns about potential cardiovascular risks associated with excessive calcium intake. For most people, a well-balanced diet rich in calcium ( see table above) from natural sources like dairy, leafy greens, and even mineral waters provides adequate nutrition without the need for supplements. Additionally, people on specific osteoporosis treatments may still require low doses of calcium and vitamin D, but this should be done under medical supervision. In general, current evidence does not support promoting calcium supplementation as a public health measure.
- Vitamin D supplements: The latest scientific evidence suggests that routine vitamin D supplementation, particularly in older adults, may not be as beneficial as previously thought. While observational studies have linked vitamin D deficiency to various health issues, including frailty and fractures, randomized controlled trials have failed to confirm the significant benefits of supplementation for most people. In fact, some studies have even suggested that vitamin D supplementation may worsen outcomes, particularly for older individuals at risk of fractures. While some individuals with very low vitamin D levels may benefit from supplementation, the general consensus is that for the majority of people, especially those who are otherwise healthy and have access to a varied diet, vitamin D supplementation may not offer the benefits that are commonly assumed. More targeted approaches based on individual needs may be more appropriate than universal recommendations.
Understanding your osteoporosis treatment options
If you're at risk for osteoporosis (weak bones), here’s a guide to help you understand your treatment options:
1. Finding the right treatment
Your doctor will consider your risk of fractures, your preferences, and the cost of treatments when deciding on the best option for you. Usually, medications that slow down bone loss are the first choice.
2. Medications to help strengthen bones
First-line options: Antiresorptive agents
1. Oral medications: Bisphosphonates
Examples: Alendronate (Fosamax), Risedronate (Actonel), Ibandronate (Boniva)
They are typically taken once a week in tablet form. These medications work by slowing down bone resorption and can reduce the risk of fractures by about 50% over a period of three to five years.
However, their protective effect is only maintained as long as the medication is being taken. Once treatment is paused, the protective benefit diminishes.
2. Intravenous (IV) medication: Zoledronate, given through a vein, especially if you’ve had a hip fracture or cannot tolerate oral bisphosphonates. Zoledronate is given once a year, and it reduces bone resorption in a much more marked manner than oral bisphosphonates.
Potential side effects: One of the most common issues with oral bisphosphonates is oesophagitis - an inflammation of the oesophagus - which can make the medication difficult to tolerate. This can lead doctors to switch patients to intravenous or subcutaneous alternatives, like zoledronic acid or denosumab, which may have fewer gastrointestinal side effects.
Very rare side effects
Long-term use of bisphosphonates and other anti-resorptive drugs has been linked to rarer, but more serious, side effects. These include osteonecrosis of the jaw (ONJ), a condition where bone tissue in the jaw dies, and atypical fractures, which are unusual and often occur in the femur or thigh. Although these side effects are extremely rare, they have been the subject of significant legal attention, particularly in the US, and have led to more cautious prescribing practices. To mitigate these risks, doctors may recommend ‘drug holidays’, allowing patients to take breaks from treatment to let the effects of medication wear off and reduce the likelihood of these complications.
In summary, bisphosphonates and other anti-resorptive drugs can significantly reduce fracture risk, but their use must be carefully considered to balance their benefits with potential risks. Regular monitoring, tailored treatment plans, and breaks from medication can help to minimise the chance of severe side effects.
Second line options:
Denosumab: A monoclonal antibody that inhibits RANKL, a protein that activates osteoclasts. It also slows bone resorption and is given once every six months with a subcutaneous injection. This will reduce fracture risk by 50 or 60 per cent.
Side effects: Low calcium levels, infections and rare bone-related side effects like osteonecrosis of the jaw. (See above)
Selective oestrogen receptor modulators (SERMs): SERMs mimic the effects of oestrogen on bone tissue, slowing bone resorption. Examples: Raloxifene (Evista)
Side effects: Increased risk of blood clots, hot flushes and leg cramps.
Hormone replacement therapy (HRT): Oestrogen therapy (often combined with progesterone) was once a first-line treatment for osteoporosis in postmenopausal women. It helps prevent bone loss by mimicking the effects of oestrogen on bone.
Side effects: Increased risk of breast cancer, stroke, blood clots and heart disease. Due to these risks, HRT is used less frequently now for osteoporosis. Treatment with HRT is typically considered for women aged 60 or younger who have low risks for the above-named side effects.
If you’re older than 60, your doctor will help you decide if continuing HRT is right for you.
3. For high fracture risk
Anabolic treatments: Anabolic (bone-building) agents stimulate the formation of new bone. They are typically used in patients with severe osteoporosis or in those who have not responded to anti-resorptive therapies. If you’re at very high risk (especially if you have fractures), your doctor may suggest drugs such as
Teriparatide (Forteo): Teriparatide is a synthetic form of parathyroid hormone (PTH) that promotes bone formation by stimulating osteoblast activity (bone-building cells). It is given as a daily subcutaneous injection.
Side effects: Nausea, leg cramps, dizziness and a small increased risk of osteosarcoma (bone cancer) in animal studies, though not definitively shown in humans.
Abaloparatide (Tymlos): Abaloparatide is another synthetic peptide that mimics parathyroid hormone-related protein (PTHrP) to stimulate bone formation.
Side effects: Similar to teriparatide, including nausea and dizziness. It may also slightly increase the risk of osteosarcoma.
Romosozumab (Evenity): Romosozumab is a monoclonal antibody that works by inhibiting sclerostin, a protein that suppresses bone formation. It is administered as a monthly subcutaneous injection.
Side effects: Joint pain, headache and a small increased risk of cardiovascular events (e.g., heart attack or stroke).
4. Other treatments
These treatments are either used in specific circumstances or still being researched for osteoporosis treatment.
Strontium Ranelate: Strontium ranelate is an experimental drug in some countries. It has both bone-building and bone-resorption-suppressing effects.
Side effects: Increased risk of heart problems and venous thromboembolism (blood clots).
Calcitonin: Calcitonin is a hormone that helps regulate calcium levels in the body and inhibits bone resorption. It can be administered via nasal spray or injection.
Side effects: Nasal irritation (with nasal spray), increased risk of cancer with long-term use.
Can electroacupuncture help to manage osteoporosis?
What is electroacupuncture? A form of acupuncture that involves applying a small electrical current to acupuncture needles - has been explored as a complementary treatment for various health conditions, including osteoporosis. While the research on electroacupuncture for osteoporosis is still limited, there is some evidence to suggest it might offer potential benefits, particularly when used alongside more conventional treatments.
Here's a breakdown of the current understanding:
Potential mechanisms of action
- Pain relief: One of the primary reasons people with osteoporosis might seek acupuncture is for pain management. Osteoporosis can cause bone pain, especially if fractures or compression occur. Electroacupuncture may help reduce pain and improve mobility by stimulating the release of endorphins and other pain-relieving chemicals in the body.
- Bone remodelling: Some studies suggest that acupuncture (including electroacupuncture) may have a direct effect on bone metabolism. It’s thought that electroacupuncture could stimulate the production of certain proteins and hormones that promote osteoblast activity (cells that build bone). Research in animals has shown that acupuncture might help stimulate bone formation, but evidence in humans is still scarce.
- Improved blood flow: Electroacupuncture may enhance circulation, which could help improve nutrient delivery to bones and tissues, potentially aiding the bone healing process and improving overall bone health.
- Regulation of hormones: There is some evidence to suggest that acupuncture can help regulate the balance of hormones like oestrogen, which plays a critical role in bone health, especially in postmenopausal women. Oestrogen deficiency is one of the key contributors to osteoporosis, so therapies that can help modulate hormonal balance may provide some benefit.
Evidence for electroacupuncture in osteoporosis
- Limited studies: A few small studies have explored the effects of acupuncture or electroacupuncture on osteoporosis, particularly in terms of reducing pain, improving mobility, and potentially enhancing bone density. For example, one study indicated that electroacupuncture may improve bone mineral density (BMD) in postmenopausal women, though the effects were modest.
- Animal studies: Some research on animals has shown that electroacupuncture can promote bone healing and stimulate osteoblast function, but these results have not been consistently replicated in human trials.
- Pain relief: There is more established evidence for acupuncture (including electroacupuncture) in managing chronic pain conditions. Since people with osteoporosis often experience significant pain from fractures or bone loss, electroacupuncture may help improve quality of life by addressing pain management.
Considerations
- Not a primary treatment: While electroacupuncture may offer some benefits, it should not be viewed as a primary treatment for osteoporosis. Standard treatments such as bisphosphonates, denosumab, or hormone replacement therapy remain the cornerstone for preventing fractures and maintaining bone density. Electroacupuncture may be considered as a complementary therapy for pain relief or overall well-being, but it is unlikely to replace pharmacological interventions.
- Consultation with healthcare providers: As with any complementary therapy, it's essential for individuals with osteoporosis to consult their healthcare provider before trying electroacupuncture. It’s especially important to ensure that acupuncture treatments are performed by a trained practitioner who understands the condition and its implications.
Conclusion:
While electroacupuncture may offer some pain relief and possibly promote bone health through various mechanisms, the evidence for its effectiveness in treating osteoporosis is still limited. It should be considered as part of a broader, comprehensive treatment plan that includes medications, diet, exercise, and other lifestyle modifications, rather than as a standalone solution. Always consult a healthcare provider before incorporating alternative therapies into an osteoporosis management plan.
Do you require gold standard osteoporosis treatment? Arrange a consultation with Dr Boecklin via her Top Doctors profile.


