Pioneering precision: Minimally invasive solutions for colorectal health
Escrito por:Minimally invasive surgery has transformed how colorectal conditions are treated, resulting in less pain, quicker recovery, and increased precision compared to traditional surgical methods.
Mr Kai Leong, distinguished consultant general and colorectal surgeon, provides a comprehensive insight into minimally invasive surgery for colorectal health, addressing key questions to help you make informed decisions about your care.

What is minimally invasive surgery?
Minimally invasive surgery refers to the use of specialised surgical techniques that allow the surgeon to operate with small incisions rather than deep or large cuts in the skin. The most common minimally invasive techniques used in colorectal surgery include:
Laparoscopy
Laparoscopy involves making small incisions, through which a laparoscope (a thin tube equipped with a high-resolution camera) and specialised surgical instruments are inserted. The laparoscope provides the surgeon with a magnified and detailed view of the internal organs and the small surgical tools allow the surgeon to perform surgery with greater precision.
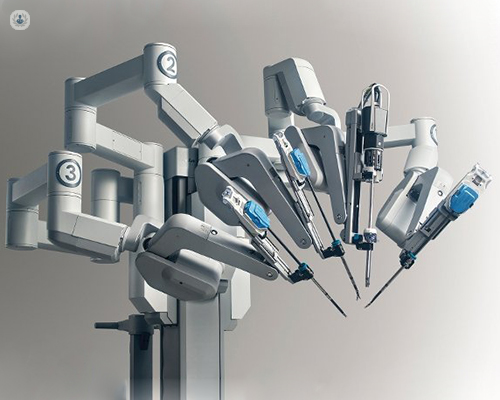
Robotic-assisted surgery
Robotic-assisted surgery uses robotic systems, such as the da Vinci surgical system, to increase precision. It involves making small incisions, through which a high-resolution camera and the robotic system’s arms are inserted. The robot offers a 3-D view that allows unparallelled resolution and accuracy. The surgeon controls the robotic arms to perform surgery and the robotic arms translate the surgeon’s hand movements into surgical movements, offering greater dexterity and stability than human hands.
How do minimally invasive solutions compare to traditional surgery?
With open surgery, large incisions are required to access the affected area, while minimally invasive techniques use incisions that are often less than an inch long. This results in less pain, less blood loss, reduced risk of infection, and a much shorter recovery time.
Patients undergoing minimally invasive surgery therefore typically spend fewer days in the hospital and return to their normal activities more quickly. Additionally, the smaller incisions result in minimal scarring, which can be an important consideration.
In terms of surgical outcomes, research has shown that minimally invasive surgery is as successful as traditional surgery for treating colorectal conditions, with the added benefit of lower complication rates.
What colorectal conditions can be treated using minimally invasive surgery?
Minimally invasive surgery is effective for a wide range of colorectal conditions, including:
- Colorectal cancer: Early and advanced-stage colorectal cancer can be treated with minimally invasive surgery to ensure precise removal of the tumour while preserving surrounding structures.
- Diverticulitis: Minimally invasive surgery can help remove affected portions of the colon in severe cases of diverticulitis, thereby reducing complications.
- Inflammatory bowel disease (IBD): Crohn’s disease and ulcerative colitis often require surgical intervention when medications are insufficient. Minimally invasive surgery can help resect diseased sections of the bowl with little impact on healthy tissue.
Each case is unique, and your surgeon will carefully assess your situation with you to determine the most appropriate approach.
Is minimally invasive colorectal surgery safe?
Yes, minimally invasive colorectal surgery is considered safe when performed by a skilled and experienced surgeon.
However, like any surgical procedure, there are potential risks and complications, such as bleeding, infection, blood clots, or injury to surrounding structures. In rare cases, your surgeon will need to convert a minimally invasive procedure to open surgery if unexpected issues arise during the operation.
For this reason, it’s essential to have a detailed discussion with your surgeon about the risks and benefits during the consultation phase. Before undergoing surgery, your surgeon will also provide specific instructions on how to prepare for surgery to reduce the likelihood of complications.
How can I maintain colorectal health after surgery?
After minimally invasive surgery, you will require regular follow-ups with your surgeon. These follow-ups will allow your surgeon to monitor your healing, address any complications, and assess the success of the procedure.
In cases of cancer, follow-ups will include imaging and blood tests to ensure that the cancer has not returned. Patients with inflammatory bowel disease will also require long-term management, including medications and lifestyle modifications such as eating a high-fibre diet, practising regular exercise, and drinking plenty of water.
Furthermore, you should also be aware of symptoms that might signal a recurrence or new colorectal issues, and report them to your surgeon promptly. Your surgeon will provide you with a personalised plan for follow-up care and guidance on treatment if needed.
If you would like to book an appointment with Mr Kai Leong, head on over to his Top Doctors profile today.


