Sindrome de asherman
What is Asherman’s syndrome?
Asherman’s syndrome or Asherman syndrome is a rare, acquired condition that refers to the presence of scar tissue in the uterus or cervix. This scar tissue causes the uterine walls to be thicker, reducing the size of the uterus, and in severe cases, the walls can sometimes fuse together. Asherman’s syndrome is also known as intrauterine adhesions (IUA).
Prognosis of Asherman’s syndrome:
Asherman’s syndrome is not life-threatening, however, some women with this condition cannot conceive or will experience recurrent miscarriages. The risk of miscarriage and stillbirth are both higher in women with Asherman’s syndrome. Women with this condition are also more at risk of suffering from bleeding during pregnancy. However, if it is treated fertility can be restored.
Symptoms of Asherman’s syndrome:
The following are the common symptoms of Asherman’s syndrome:
- Light periods
- No periods
- Irregular periods
- Menstruation pain without any bleeding (this suggests that scar tissue is blocking the exit of the uterus, preventing blood from leaving during menstruation)
- Recurrent miscarriages
- Difficulty conceiving
Medical tests to diagnose Asherman’s syndrome:
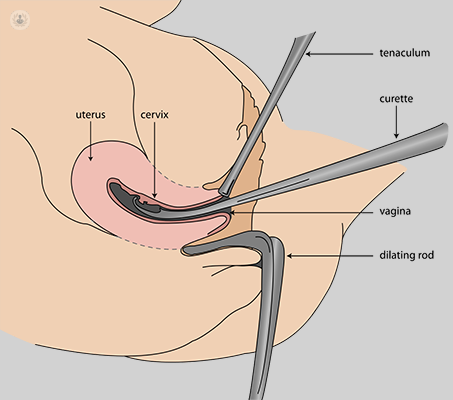
A thorough medical history will be taken and a physical examination performed, however, it is very uncommon that adhesions are found in a physical examination. A first test will usually involve a blood test to rule out other possible conditions. You will also have an ultrasound to assess the uterine lining. The most reliable method of diagnosing Asherman’s syndrome is hysteroscopy. This involves inserted a hysteroscope through the cervix to see the uterus. You may also have a hysterosalpingogram (HSG) which uses contrast dye to show blockages on an X-ray.
What are the causes of Asherman’s syndrome?
Most cases of Asherman’s syndrome result after a dilation and curettage (D and C) procedure which is usually carried out after an incomplete miscarriage, as a means of pregnancy termination or if the placenta is retained after delivery. The risk of developing this condition increases with the number of D and C procedures had. Other causes of Asherman’s syndrome include severe pelvic infections and other forms of pelvic surgery (e.g. caesarean section and fibroid or polyp removal).
Can Asherman’s syndrome be prevented?
The main way to prevent Asherman’s syndrome is to avoid having a D and C procedure. Instead, medical evacuation can be had instead following an incomplete miscarriage, retained placenta or a post-delivery haemorrhage. If a D and C is needed, then an ultrasound should be used to guide the surgeon and to reduce the risk of damage to the uterus.
Treatments for Asherman’s syndrome:
Asherman’s syndrome can be treated surgically, cutting and removing the adhesions or scar tissue. This can be done with a hysteroscopy to avoid invasive, open surgery. This requires general anaesthesia and after surgery, oestrogen may be given to improve the quality of the uterine lining. Adhesions can recur following surgery, so it may be necessary to wait for up to 12 months before trying to conceive.
Which type of specialist treats Asherman’s syndrome?
Obstetricians and gynaecologists treat Asherman’s syndrome.