Coronavirus guidance for lupus patients
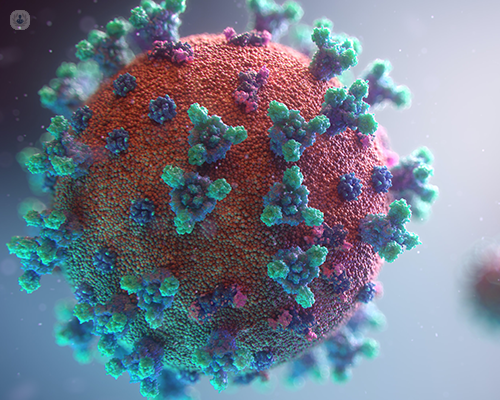
Written in association with:Lupus patients face an additional risk from the coronavirus COVID-19 virus. People with lupus are considered to be immunocompromised and could be at higher risk for infections in general because of their underlying disease and some of the medications prescribed for this condition. Consultant rheumatologist Dr Syed Asad Hussain explains this risk and provides you with professional guidance on how to approach lupus medication and work during the pandemic.
Is coronavirus more dangerous for people with lupus?
Risk of contracting the virus
The risk of lupus patients contracting the virus depends on the same factors that the rest of the population face regarding virus transmission. This means that it’s vital to:
- Observe social distancing.
- Wear full face masks.
- Use common sense as much as possible when considering your potential exposure to the virus.
You can receive reliable and continuously updated guidance from the NHS and Public Health England.
Risk of severe COVID symptoms
While the risk of transmission is the same as with the rest of the country, lupus patients are at risk of developing a much more aggressive response because of the background medical problems associated with lupus. Additionally, if a lupus patient contracts the virus, there is the potential that medication can worsen symptoms.
Should lupus patients with coronavirus continue their medication?
Depending on the nature of symptoms, a patient might be asked to immediately stop their medication. This must be done with guidance and the aim is to contact your doctor or rheumatologist as a matter of urgency.
Any patient who develops flu-like symptoms must seek advice by calling 111. More importantly, they should contact their rheumatologist in case of symptoms.
Can lupus drugs treat coronavirus? Is there any research on this?
The only medication which has proven to improve COVID symptoms (mainly the respiratory reaction caused by the coronavirus) is dexamethasone, which is a steroid preparation.
There are certain scientific and biological explanations regarding the use of hydroxychloroquine, but no formal conclusions have been reached in research so far. There are ongoing trials and research on a number of agents. The principle is to wait for formal recommendations based on clinical evidence and robust trials before any patients consider alternative treatments. This will need to be done under the guidance of a rheumatologist who has a much clearer understanding and experience of dealing with the virus.
If a patient with lupus works with children, such as in a school, is it safe for them to return to work?
The UK Government has concluded that it’s safe for teachers and assistants to return to school and provided formal guidance on safety at the workplace. This guidance ranges from class sizes and movement in between classes, to the new terminology 'bubble'.
However, it would be reasonable for patients with lupus to have a formal discussion with their rheumatologist before engaging with work. Recommendations from the government concerning the UK population can provide general guidance, but individual situations need to be taken into account. A rheumatologist can provide guidance for lupus patients and also provide necessary communication to improve on safety if required.
Is it safe for lupus patients to visit their doctor’s clinic?
Yes, patients can be invited to the clinic. Having said that, the current situation is that video or remote consultations are encouraged. Rheumatologists now have an abundance of experience dealing with patients with complex issues such as lupus by video consultation.
In some cases, the doctor may decide that the patient should come in for a face-to-face assessment. In such situations, there are numerous safety precautions to greatly minimise the risk of virus transmission.
How can a patient with lupus remain safe during the COVID-19 era?
Safety can be broadly described in three main ways:
- Firstly, common sense is the prevailing principle. Everyone should adhere to recommendations made nationally and to look at their personal circumstances when making decisions.
- Secondly, rheumatologists can provide ample support with recommendations, education and review of medications and disease activity. Keep up communication with your rheumatologist.
- Finally and equally important, it’s vital that patients with lupus or any other autoimmune disease are very knowledgeable about their condition and know when to ask for help.
Don't delay in asking for help. We (rheumatologists) welcome earlier intervention and are here to provide experience and a personalised management plan for you.
Dr Hussain provides first-class rheumatology care. Visit his Top Doctors profile to learn how his leading expertise can benefit you, and arrange a consultation.


