Understanding pancreatic cancer
Written in association with:Pancreatic cancer is one of the most challenging malignancies to diagnose and treat, often presenting with few specific symptoms until it has reached advanced stages. Early detection is thus crucial for improving patient outcomes.
Mr Nikolaos Chatzizacharias, renowned consultant hepato-pancreato-biliary and liver transplant surgeon, will explore the symptoms and staging of pancreatic cancer, along with the different treatment options available, including surgery.
What is pancreatic cancer?
The pancreas is a large gland situated behind the stomach in the back of the abdomen. It produces hormones, including insulin, which regulates blood sugar levels, as well as pancreatic juices that contain vital enzymes.
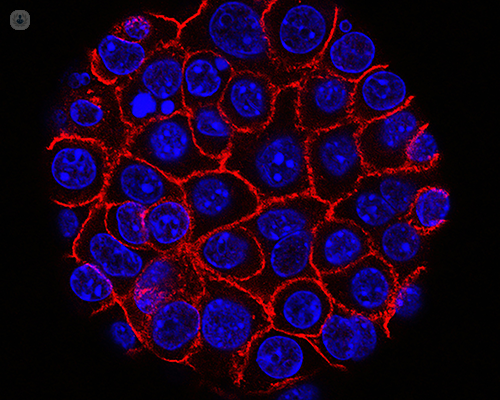
Normally, cells in the body, including those in the pancreas, grow in a controlled manner. However, sometimes, this control breaks down, causing cells to begin growing uncontrollably. These cells subsequently create a mass referred to as cancer.
There are different types of pancreatic cancer. The most prevalent types of pancreatic cancer, which make up about 80% of all cases, originate from the cells lining the pancreatic ducts and are referred to as pancreatic ductal adenocarcinoma.
What are the symptoms of pancreatic cancer?
In its early stages, pancreatic cancer typically doesn’t cause many noticeable symptoms, making it difficult to diagnose. If symptoms do present, they may include:
- loss of appetite
- indigestion
- unintentional weight loss
- nausea or vomiting
- abdominal pain or back pain
- bowel issues, such as constipation, pale or greasy floating stools, or diarrhoea
- jaundice or itchy skin
- new onset of blood sugar issues (diabetes) or problems in regulating sugar levels (in people with existing diabetes)
How is pancreatic cancer diagnosed?
When you present symptoms that raise concerns for pancreatic cancer, the initial tests typically include blood tests. These are often followed by an ultrasound scan. The most effective test for diagnosing pancreatic cancer is a CT scan with contrast, administered through a cannula in the arm. Other tests, such as MRI or PET scans, may also be utilised to help in diagnosis and staging. If the diagnosis remains unclear, an endoscopic ultrasound and a biopsy of the mass will be necessary.
Additionally, it’s essential to classify cancers by stage at the time of diagnosis. Your multidisciplinary cancer team, which will consist of specialists from various fields (including oncologists, surgeons, and radiologists) will create an individualised treatment plan based on your specific cancer stage. Among the different staging systems for pancreatic cancer, the most common one divides cancer into four stages. In stage 4, the cancer has metastasised, meaning it has spread to distant organs in the body.
Following cancer staging, the system widely-used for guiding treatment decisions in pancreatic cancer is from the USA National Comprehensive Cancer Network, which categorises pancreatic cancers into those confined to the pancreas and those that are metastatic.
Cancers that haven’t metastasised are further classified as "resectable," "borderline resectable," or "locally advanced", based on the tumour's involvement with the major blood vessels near the pancreas. Tumours that don’t involve any vessels, or only lightly touch the major veins, are considered "resectable." If the tumour involves the large vessels more extensively, it’s classified as either "borderline resectable" or "locally advanced," based on the extent of involvement.
What treatment options are available for pancreatic cancer?
Treatment options for pancreatic cancer include surgery, chemotherapy, radiotherapy, and various clinical trials. The choice of treatment will depend on the stage of your cancer, along with your overall health and medical history. In certain cases, treatments may be given in combination.
For pancreatic cancer classified as “resectable,” the first-line treatment is surgery, followed by chemotherapy. When chemotherapy is given after surgery, this is known as “adjuvant chemotherapy.”
In instances where pancreatic cancer is categorised as “borderline resectable” or “locally advanced,” chemotherapy is the first treatment. This is then known as “neoadjuvant chemotherapy.” After three to six months of chemotherapy (as determined by your multidisciplinary cancer team), further investigations will be conducted. Based on these results, your hepato-pancreato-biliary surgeon will assess whether surgery is possible, which will need to be scheduled within 4 to 6 weeks following the completion of neoadjuvant treatment.
What are the different types of surgical options?
There are three main types of operations for pancreatic cancer, based on the specific area of the pancreas affected and the involvement of nearby organs or major blood vessels.
Pancreaticoduodenectomy (classical or pylorus-preserving)
A pancreaticoduodenectomy is the standard procedure for tumours situated in the head of the pancreas. During this surgery, your hepato-pancreato-biliary surgeon will remove the head of the pancreas, the duodenum, 15-20 cm of the small intestine, the gallbladder, and a portion of the bile duct.
In the classical pancreaticoduodenectomy, the distal portion of the stomach will also be removed, whereas in the pylorus-preserving pancreaticoduodenectomy, the stomach will be left intact. Afterward, the remaining pancreas, bile duct, and stomach will be reconnected to the intestine.
Distal pancreatectomy and splenectomy
A distal pancreatectomy and splenectomy is the usual surgery performed for tumours in the body and tail of the pancreas. During this surgery, your hepato-pancreato-biliary surgeon will remove the tail and body of the pancreas, as well as the surrounding tissues.
Additionally, the spleen will also be taken out. This is done for two reasons: first, the blood vessels supplying the spleen are positioned adjacent to the body and tail of the pancreas, and second, the lymph nodes that must be removed to eliminate any cancer are closely linked to the spleen.
Total pancreatectomy and splenectomy
In some cases, a total pancreatectomy will be required to ensure the complete removal of pancreatic cancer. This procedure integrates aspects of both the pancreaticoduodenectomy and the distal pancreatectomy with splenectomy.
Why is selecting your doctors important for a good outcome?
The management of pancreatic cancer is a complex undertaking that is, therefore, better delivered by specialist multidisciplinary teams that regularly manage such cases. Furthermore, evidence supports that surgery for pancreatic cancer achieves better outcomes when the operation is performed in a high-volume centre, with pancreatic surgery having been centralised in the UK for many years now.
However, even with measures within the speciality, not all aspects of surgical treatment are offered everywhere, and expertise can vary widely within specialist centres and surgical teams. These variations in experience are most notable in cases of "borderline resectable" and "locally advanced" tumours, when operating after neoadjuvant chemotherapy and on major vessels is crucial for a successful outcome.
During these operations, techniques to separate the tumour from large veins and arteries, or to resect these vessels and reconnect them to the circulation, are usually required and are not widely practised. Therefore, identifying and selecting a surgeon with substantial experience is highly recommended.
If you would like to book an appointment with Mr Nikolaos Chatzizacharias, head on over to his Top Doctors profile today.


