What is ulcerative colitis?
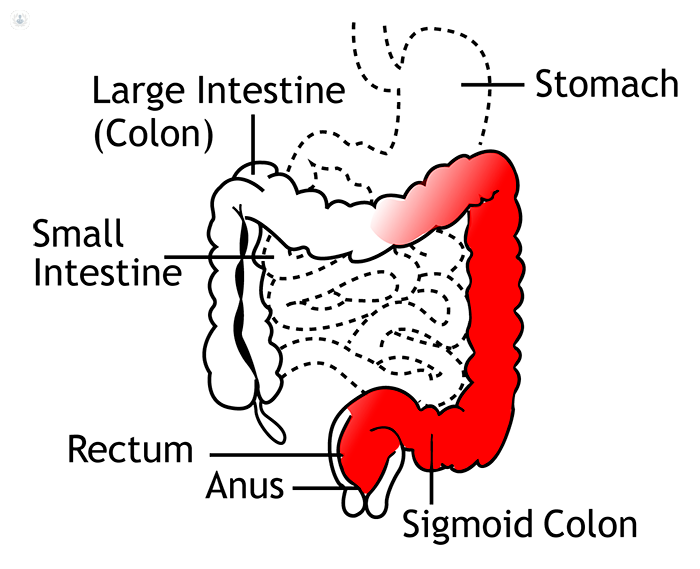
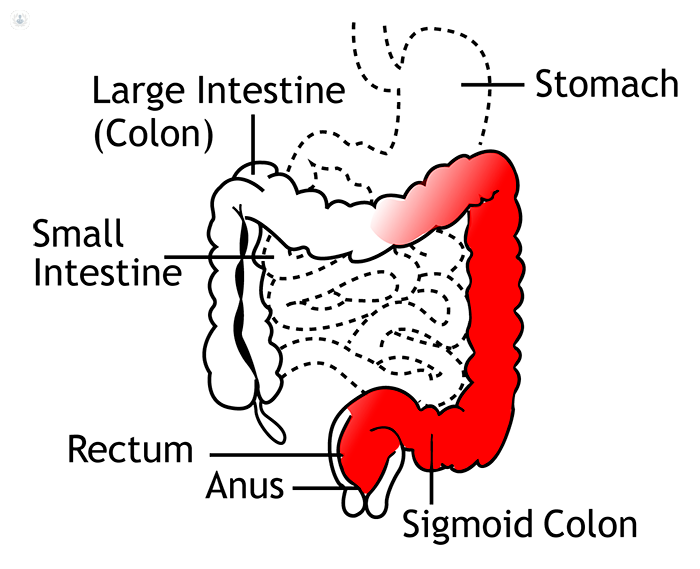
Ulcerative colitis is a condition where the large intestine and rectum become inflamed and eventually produce ulcers. It is a type of inflammatory bowel disease, along with Crohn’s disease. Inflammatory bowel disease affects more than 620,000 people in the UK .
Can it be cured?
Ulcerative colitis is a long-term condition, which means it can’t be cured. Instead, treatment focusses on managing the symptoms, and achieving “remission”, where no symptoms occur.
This doesn’t mean that symptoms can’t come back – ulcerative colitis is a fluctuating condition involving “flare-ups” (see below).
Symptoms of ulcerative colitis
The main symptoms of ulcerative colitis include:
- diarrhoea, often containing blood
- stomach pain and rectal pain
- fequently needing to go to the toilet
- weight loss
- fatigue
Ulcerative colitis is characterised by “flare-ups”, where symptoms worsen for a period of time, and you can experience symptoms in other parts of the body. These can include:
- mouth ulcers
- a high temperature
- painful and swollen joints
- irritated eyes
Everyone experiences ulcerative colitis differently. With the right treatment and self-management, some people can experience long periods of “remission” where you only experience mild symptoms, or even none at all.
Diagnosis
Diagnosis will usually involve a combination of:
- taking a stools sample to rule out other conditions such as an infection or colon
- blood tests to rule out anaemia or inflammation
- sigmoidoscopy or colonoscopy to see inside your large intestine
Sometimes the doctor might need to do an X-ray to check if there are serious complications, but this is much less common.
What causes ulcerative colitis?
It’s not clear exactly what causes ulcerative colitis. Many health professionals now think that it could be an autoimmune condition, involving the immune system mistakenly attacking healthy cells. This may be triggered by an infection in the large intestine.
However, other factors appear to play a role:
- you’re more likely to have the condition if a family member has had it
- having certain genes makes you more likely to have the condition
- the condition is more common in places with better sanitation
Ulcerative colitis therefore seems to be caused by a combination of genetic and environmental factors.
Treatment
Treatment for ulcerative colitis includes lifestyle and diet changes, medication, and in very rare cases, surgery.
Lifestyle changes
For some people, making changes to their diet can help control the symptoms and reduce the frequency of “flare-ups”. Some helpful changes can include:
- Making sure you stay hydrated by drinking plenty of liquids through the day
- Making sure you have a well-balanced diet with all the vitamins and minerals you need, possibly with the aid of supplements
- Avoiding foods you have any intolerance to (e.g. avoiding dairy products if you’re lactose intolerant)
- Eating smaller, more frequent meals, rather than a few large meals
Medication
Your doctor may prescribe a combination of drugs to achieve different goals, including:
- Anti-inflammatory drugs such as aminosalicylates and corticosteroids
- Immunosuppressants usually used to treat flare-ups, or to treat patients who haven’t responded to anti-inflammatory drugs
Surgery
Surgery is generally only recommended when a patient hasn’t responded to medication, or are experiencing severe flare-ups that significantly affect their day to day life.
Surgery will involve removing the colon, and replacing its function with an ileostomoy or ileo-anal pouch. This results in a complete cure of the condition.
08-28-2013 11-14-2023Ulcerative colitis
Dr Carlo Nunes - Gastroenterology
Created on: 08-28-2013
Updated on: 11-14-2023
Edited by: Conor Dunworth
What is ulcerative colitis?
Ulcerative colitis is a condition where the large intestine and rectum become inflamed and eventually produce ulcers. It is a type of inflammatory bowel disease, along with Crohn’s disease. Inflammatory bowel disease affects more than 620,000 people in the UK .
Can it be cured?
Ulcerative colitis is a long-term condition, which means it can’t be cured. Instead, treatment focusses on managing the symptoms, and achieving “remission”, where no symptoms occur.
This doesn’t mean that symptoms can’t come back – ulcerative colitis is a fluctuating condition involving “flare-ups” (see below).
Symptoms of ulcerative colitis
The main symptoms of ulcerative colitis include:
- diarrhoea, often containing blood
- stomach pain and rectal pain
- fequently needing to go to the toilet
- weight loss
- fatigue
Ulcerative colitis is characterised by “flare-ups”, where symptoms worsen for a period of time, and you can experience symptoms in other parts of the body. These can include:
- mouth ulcers
- a high temperature
- painful and swollen joints
- irritated eyes
Everyone experiences ulcerative colitis differently. With the right treatment and self-management, some people can experience long periods of “remission” where you only experience mild symptoms, or even none at all.
Diagnosis
Diagnosis will usually involve a combination of:
- taking a stools sample to rule out other conditions such as an infection or colon
- blood tests to rule out anaemia or inflammation
- sigmoidoscopy or colonoscopy to see inside your large intestine
Sometimes the doctor might need to do an X-ray to check if there are serious complications, but this is much less common.
What causes ulcerative colitis?
It’s not clear exactly what causes ulcerative colitis. Many health professionals now think that it could be an autoimmune condition, involving the immune system mistakenly attacking healthy cells. This may be triggered by an infection in the large intestine.
However, other factors appear to play a role:
- you’re more likely to have the condition if a family member has had it
- having certain genes makes you more likely to have the condition
- the condition is more common in places with better sanitation
Ulcerative colitis therefore seems to be caused by a combination of genetic and environmental factors.
Treatment
Treatment for ulcerative colitis includes lifestyle and diet changes, medication, and in very rare cases, surgery.
Lifestyle changes
For some people, making changes to their diet can help control the symptoms and reduce the frequency of “flare-ups”. Some helpful changes can include:
- Making sure you stay hydrated by drinking plenty of liquids through the day
- Making sure you have a well-balanced diet with all the vitamins and minerals you need, possibly with the aid of supplements
- Avoiding foods you have any intolerance to (e.g. avoiding dairy products if you’re lactose intolerant)
- Eating smaller, more frequent meals, rather than a few large meals
Medication
Your doctor may prescribe a combination of drugs to achieve different goals, including:
- Anti-inflammatory drugs such as aminosalicylates and corticosteroids
- Immunosuppressants usually used to treat flare-ups, or to treat patients who haven’t responded to anti-inflammatory drugs
Surgery
Surgery is generally only recommended when a patient hasn’t responded to medication, or are experiencing severe flare-ups that significantly affect their day to day life.
Surgery will involve removing the colon, and replacing its function with an ileostomoy or ileo-anal pouch. This results in a complete cure of the condition.


All you need to know about J-pouch surgery
By Mr Talvinder Gill
2024-11-21
J-pouch surgery can offer patients with serious bowel disease, such as ulcerative colitis improved outcomes and a life without the need for a stoma. Renowned consultant colorectal surgeon Mr Talvinder Gill gives a detailed guide to J-pouch surgery in this informative article and describes how he employs a single incision technique to improve safety in his practice. See more


Preparing for a colonoscopy
By Mr David McArthur
2024-11-20
A colonoscopy looks for changes inside your bowels and is a diagnostic procedure that can find what's causing symptoms in the area. There’s a certain amount of preparation required from patients. So, what's involved? Mr David McArthur, a leading general and colorectal surgeon in Birmingham, provides a detailed answer in this informative article. See more


IBD: Crohn's disease (CD) vs ulcerative colitis (UC)
By Dr Evangelos Russo
2024-11-20
Of the causes of inflammatory bowel disease, Crohn’s disease and ulcerative colitis are the two most common. Dr Evangelos Russo, an expert gastroenterologist, shares his expertise about these two conditions and clarifies how common they are, their symptoms, how doctors distinguish between the two, which is more serious, as well as the available treatments for both. See more


Minimally-invasive techniques in gastroenterology
By Professor Owen Epstein
2024-11-20
When it comes to diagnosing gastrointestinal conditions such as ulcerative colitis or diverticular disease, there are minimally invasive techniques that are used to make that diagnosis. Read more from our expert gastroenterologist Professor Owen Epstein on the different tools used and what the future holds for technologies in gastroenterology. See more
Experts in Ulcerative colitis
-
Dr Peter Irving
GastroenterologyExpert in:
- Inflammatory bowel disease (IBD)
- Crohn's disease
- Ulcerative colitis
- Irritable bowel syndrome (IBS)
- Gastroscopy
- Colonoscopy
-
Mr Richard Lovegrove
Colorectal surgeryExpert in:
- Ulcerative colitis
- Colorectal cancer
- Crohn's disease
- Anal fistula
- Piles (haemorrhoids)
- Colonoscopy
-
Dr Shameer Mehta
GastroenterologyExpert in:
- Radiotherapy side effects
- Inflammatory bowel disease (IBD)
- Clinical nutrition
- Crohn's disease
- Ulcerative colitis
- Intestinal failure
-
Dr Farooq Rahman
GastroenterologyExpert in:
- Inflammatory bowel disease (IBD)
- Crohn's disease
- Ulcerative colitis
- Irritable bowel syndrome (IBS)
- Colonoscopy
- Coeliac disease
-
Professor James Lindsay
GastroenterologyExpert in:
- Inflammatory bowel disease (IBD)
- Endoscopy
- Colonoscopy
- Crohn's disease
- Irritable bowel syndrome (IBS)
- Ulcerative colitis
- See all

The Princess Grace Hospital - part of HCA Healthcare
The Princess Grace Hospital - part of HCA Healthcare
The Princess Grace Hospital, 42-52 Nottingham Pl, W1U 5NY
No existe teléfono en el centro.
By using the telephone number provided by TOP DOCTORS, you automatically agree to let us use your phone number for statistical and commercial purposes. For further information, read our Privacy Policy
Top Doctors

The Blackheath Hospital - part of Circle Health Group
The Blackheath Hospital - part of Circle Health Group
40-42 Lee Terrace, Blackheath, London SE3 9UD
No existe teléfono en el centro.
By using the telephone number provided by TOP DOCTORS, you automatically agree to let us use your phone number for statistical and commercial purposes. For further information, read our Privacy Policy
Top Doctors

The Sloane Hospital - part of Circle Health Group
The Sloane Hospital - part of Circle Health Group
125 Albemarle Rd, Beckenham BR3 5HS
No existe teléfono en el centro.
By using the telephone number provided by TOP DOCTORS, you automatically agree to let us use your phone number for statistical and commercial purposes. For further information, read our Privacy Policy
Top Doctors
-
The Princess Grace Hospital - part of HCA Healthcare
The Princess Grace Hospital, 42-52 Nottingham Pl, W1U 5NY, Central LondonExpert in:
- Cancer
- General Surgery
- Orthopaedic surgery
- Robotic Surgery
- Intensive care
- Sports Medicine
-
The Blackheath Hospital - part of Circle Health Group
40-42 Lee Terrace, Blackheath, London SE3 9UD, East LondonExpert in:
- Vascular Surgery
- Cardiology
- Bariatric Surgery
- Colorectal surgery
- Endocrine Surgery
- General Surgery
-
The Sloane Hospital - part of Circle Health Group
125 Albemarle Rd, Beckenham BR3 5HS , South LondonExpert in:
- Abdominal ultrasound
- Vascular Surgery
- Cardiology
- Colorectal surgery
- Endocrine Surgery
- General Surgery
- See all
- Most viewed diseases, medical tests, and treatments
- Migraine
- Paediatric rheumatology
- Autoimmune diseases
- Joint pain
- Child nutrition
- Nutrition
- Weight loss injections
- Nipple discharge
- Abdominal pain
- Endovenous laser treatment (EVLA)








