What is dialysis?
Dialysis is a treatment that extracts toxins and excess water from the blood. It acts as a substitute for the kidneys in patients whose own kidneys are not working.
The main function of the kidneys is to remove toxins and liquid from the blood, as the accumulation of waste products in the blood is dangerous. During dialysis, the machine helps the kidneys perform their function. Hence, during the process:
- excess salt, water and waste products are removed so that they do not accumulate in the body
- adequate levels of minerals and vitamins are maintained in the body
Dialysis also helps to control blood pressure and helps in the production of red blood cells.
There are two types of dialysis: haemodialysis and peritoneal dialysis.
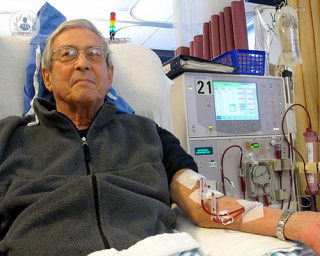
Haemodialysis
This is the typical dialysis treatment, characterised by use of an artificial membrane. The blood is cleansed by an artificial kidney, which removes excess water, residues and toxins, then returns the blood to the body. Each session lasts around four hours.
Peritoneal dialysis
Peritoneal dialysis is characterised by use of a natural membrane (the patient’s peritoneum). It consists in removing waste and excess liquid through a tube (catheter) towards a specific part of the abdomen. After a while, the liquid containing the filtered-out waste products is directed outside of the abdomen and discarded. We can distinguish between continuous ambulatory peritoneal dialysis (between 30 and 40 meticulous sessions, four times a day) and automated peritoneal dialysis (performed at night while the patient is asleep).
Why is it done?
Dialysis is performed in patients with renal insufficiency, which is the final phase of chronic kidney disease. This occurs when the kidneys are no longer capable of performing their excretory function and are functioning at between 10 and 15 per cent of their normal levels. The therapy is considered a stop-gap measure until a kidney transplant can be performed; sometimes, it is the only supportive therapy available in cases where transplant is not a viable option.
Some kidney diseases that may require dialysis are: uraemic encephalopathy, pericarditis, acidosis and hyperkalaemia.
What does it involve?
Both types of dialysis have the same goal: to substitute some of the kidney’s functions. Hence, the goal is to eliminate waste products and excess liquid, and equilibrate the amount of electrolytes and other substances.
During dialysis, a semipermeable membrane separates the blood from the dialysis liquid. The membrane only allows certain substances, e.g. waste products, water, electrolytes, to pass from the blood to the dialysis liquid via a process called diffusion.
In dialysis, it is the dialysis liquid which makes it possible to eliminate waste products from the blood. In addition, it contains substances to help correct the misbalances caused by renal insufficiency.
How to prepare for dialysis
Preparation depends on which dialysis method is selected by the nephrologist. Depending on the choice, you may or may not be fitted with a catheter through which the dialysis liquid will be introduced.
Furthermore, it is always advisable to:
- pursue a healthy diet, low in potassium and proteins (a kidney diet)
- continue with your prescribed kidney medication
- rest adequately and sleep before and during dialysis
Care following the intervention
After dialysis, it is normal to feel tired, weak and even to tremble; hence it is recommended to rest when you return home. However, you can resume your everyday activities as soon as you feel better. You must also wash with soap and water the area through which dialysis was introduced, and be careful with the scabs that form.
Alternatives to this treatment
The alternative to dialysis is a kidney transplant. One of the requirements of a kidney transplant is that the patient’s kidney is compatible with the donor’s kidney. A kidney transplant operation usually takes approximately three hours to perform.
02-08-2013 10-11-2023Dialysis
Dr Andrew Palmer - Nephrology
Created on: 02-08-2013
Updated on: 10-11-2023
Edited by: Sophie Kennedy
What is dialysis?
Dialysis is a treatment that extracts toxins and excess water from the blood. It acts as a substitute for the kidneys in patients whose own kidneys are not working.
The main function of the kidneys is to remove toxins and liquid from the blood, as the accumulation of waste products in the blood is dangerous. During dialysis, the machine helps the kidneys perform their function. Hence, during the process:
- excess salt, water and waste products are removed so that they do not accumulate in the body
- adequate levels of minerals and vitamins are maintained in the body
Dialysis also helps to control blood pressure and helps in the production of red blood cells.
There are two types of dialysis: haemodialysis and peritoneal dialysis.
Haemodialysis
This is the typical dialysis treatment, characterised by use of an artificial membrane. The blood is cleansed by an artificial kidney, which removes excess water, residues and toxins, then returns the blood to the body. Each session lasts around four hours.
Peritoneal dialysis
Peritoneal dialysis is characterised by use of a natural membrane (the patient’s peritoneum). It consists in removing waste and excess liquid through a tube (catheter) towards a specific part of the abdomen. After a while, the liquid containing the filtered-out waste products is directed outside of the abdomen and discarded. We can distinguish between continuous ambulatory peritoneal dialysis (between 30 and 40 meticulous sessions, four times a day) and automated peritoneal dialysis (performed at night while the patient is asleep).
Why is it done?
Dialysis is performed in patients with renal insufficiency, which is the final phase of chronic kidney disease. This occurs when the kidneys are no longer capable of performing their excretory function and are functioning at between 10 and 15 per cent of their normal levels. The therapy is considered a stop-gap measure until a kidney transplant can be performed; sometimes, it is the only supportive therapy available in cases where transplant is not a viable option.
Some kidney diseases that may require dialysis are: uraemic encephalopathy, pericarditis, acidosis and hyperkalaemia.
What does it involve?
Both types of dialysis have the same goal: to substitute some of the kidney’s functions. Hence, the goal is to eliminate waste products and excess liquid, and equilibrate the amount of electrolytes and other substances.
During dialysis, a semipermeable membrane separates the blood from the dialysis liquid. The membrane only allows certain substances, e.g. waste products, water, electrolytes, to pass from the blood to the dialysis liquid via a process called diffusion.
In dialysis, it is the dialysis liquid which makes it possible to eliminate waste products from the blood. In addition, it contains substances to help correct the misbalances caused by renal insufficiency.
How to prepare for dialysis
Preparation depends on which dialysis method is selected by the nephrologist. Depending on the choice, you may or may not be fitted with a catheter through which the dialysis liquid will be introduced.
Furthermore, it is always advisable to:
- pursue a healthy diet, low in potassium and proteins (a kidney diet)
- continue with your prescribed kidney medication
- rest adequately and sleep before and during dialysis
Care following the intervention
After dialysis, it is normal to feel tired, weak and even to tremble; hence it is recommended to rest when you return home. However, you can resume your everyday activities as soon as you feel better. You must also wash with soap and water the area through which dialysis was introduced, and be careful with the scabs that form.
Alternatives to this treatment
The alternative to dialysis is a kidney transplant. One of the requirements of a kidney transplant is that the patient’s kidney is compatible with the donor’s kidney. A kidney transplant operation usually takes approximately three hours to perform.


What conditions can dialysis help to manage and when is it needed?
By Dr Andrew Palmer
2025-02-01
The kidneys are responsible for filtering waste substances out of our blood and expelling them as urine. However, kidney failure can mean that a patient needs to have their blood filtered by a machine to survive. This is called dialysis. Respected nephrologist Dr Andrew Palmer is here to answer all the questions you may have about this procedure. See more

How does haemodialysis (kidney dialysis) work?
By Dr Ravi Rajakariar
2025-02-01
Leading consultant nephrologist, Dr Ravi Rajakariar explains how haemodialysis works, and what patients should expect. See more


Kidney transplant: how are donors and recipients matched?
By Dr David Game
2025-02-01
Kidneys are the most commonly donated organ around the world, and every year, thousands of people give one of theirs to either a friend, relative or someone they don’t know. For a successful kidney transplant to go underway, donors and recipients must have compatible blood types - but that doesn’t always mean they need to have the same blood type. Dr David Game, a leading nephrologist from London, explains more. See more


Renal failure: dialysis vs. kidney transplant
By Dr Andrew Palmer
2025-01-31
Renal failure is a potentially life-threatening consequence of long-term kidney disease. When the kidneys fail, there are two key treatments to save the patient and keep their blood filtered. Dr Andrew Palmer explains the pros and cons of dialysis and kidney transplants. See more
Experts in Dialysis
-
Dr Ravi Rajakariar
NephrologyExpert in:
- Kidney transplantation
- Hypertension (high blood pressure)
- Diabetic nephropathy
- Dialysis
- Nephropathy (Kidney disease)
- Lupus
-
Dr Andrew Palmer
NephrologyExpert in:
- Chronic kidney disease
- Nephropathy (Kidney disease)
- Urinary tract infection
- Acute kidney injury (AKI)
- Dialysis
- Kidney transplantation
-
Dr David Game
NephrologyExpert in:
- Kidney transplantation
- Chronic kidney disease
- Dialysis
- Hypertension (high blood pressure)
- Acute kidney injury (AKI)
- Kidney stones
-
Dr Stephen McAdoo
NephrologyExpert in:
- Vascular disease
- Haematuria (blood in the urine)
- Chronic kidney disease
- Proteinuria (protein in the urine)
- Nephropathy (Kidney disease)
- Dialysis
-
Dr James Tomlinson
NephrologyExpert in:
- Acute kidney injury (AKI)
- Chronic kidney disease
- Dialysis
- Hypertension (high blood pressure)
- Vascular disease
- Acute kidney failure
- See all

The Lister Hospital - part of HCA Healthcare
The Lister Hospital - part of HCA Healthcare
Chelsea Bridge Road, London
No existe teléfono en el centro.
By using the telephone number provided by TOP DOCTORS, you automatically agree to let us use your phone number for statistical and commercial purposes. For further information, read our Privacy Policy
Top Doctors

Cleveland Clinic Portland Place Outpatient Centre
Cleveland Clinic Portland Place Outpatient Centre
24 Portland Place, W1B 1LU
No existe teléfono en el centro.
By using the telephone number provided by TOP DOCTORS, you automatically agree to let us use your phone number for statistical and commercial purposes. For further information, read our Privacy Policy
Top Doctors

The Outpatients and Diagnostic Centre at 30 Devonshire Street (HCA)
The Outpatients and Diagnostic Centre at 30 Devonshire Street (HCA)
30 Devonshire St, London W1G 6PU
No existe teléfono en el centro.
By using the telephone number provided by TOP DOCTORS, you automatically agree to let us use your phone number for statistical and commercial purposes. For further information, read our Privacy Policy
Top Doctors
-
The Lister Hospital - part of HCA Healthcare
Chelsea Bridge Road, London , Central LondonExpert in:
- Cancer
- Cardiology
- Orthopaedic surgery
- Pregnancy
- Physiotherapy
- Women’s health
-
Cleveland Clinic Portland Place Outpatient Centre
24 Portland Place, W1B 1LU, Central LondonExpert in:
- Diagnosis of Cancer
- Diagnostics
- Women’s health
- Sports Medicine
- General practice
- Health check up
-
The Outpatients and Diagnostic Centre at 30 Devonshire Street (HCA)
30 Devonshire St, London W1G 6PU, Central LondonExpert in:
- Orthopaedic surgery
- Orthopaedic spinal surgery
- Musculoskeletal pain
- Musculoskeletal ultrasound
- Spinal stenosis
- Spinal injections
- See all
- Most viewed diseases, medical tests, and treatments
- Cardiovascular disease
- Kidney stones
- Metabolic disorder
- Robotic surgery
- Hypertension (high blood pressure)
- Diabetes
- Atherosclerotic renal disease
- Pregnancy and kidney disease
- Kidney cancer
- Diabetic nephropathy








