Spina bifida
Mr Bassel Zebian - Neurosurgery
Created on: 11-13-2012
Updated on: 07-28-2023
Edited by: Sophie Kennedy
What is spina bifida?
Spina bifida is a brain birth defect of the spine or spinal cord caused by a defect of the neural tube (the embryonic structure that becomes the foetal brain and spinal cord as well as in the tissues that contain them).
It tends to start in the first month of pregnancy in cases where the spinal cord doesn’t close properly. The neural tube tends to be formed during the first stages of pregnancy and closes 28 days after conception.
There are two different types of spina bifida:
- Spina bifida occulta, where there is a small defect or opening in one or more vertebrae. It normally comes with neurological symptoms (lower limb weakness, atrophy, low sensitivity, or an alteration in reflexes), genitourinary symptoms (incontinence or urinary retention), and orthopaedic symptoms (foot deformities or changes in foot size).
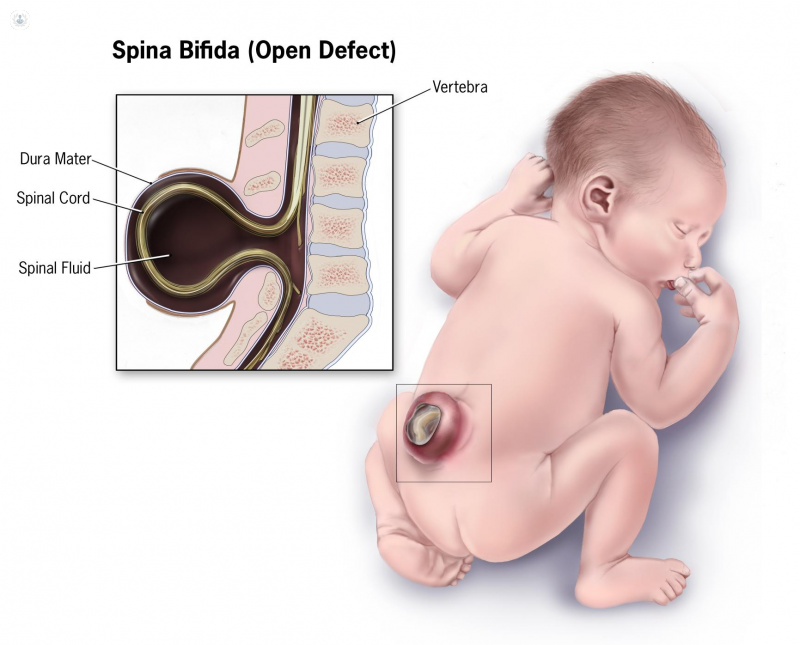
- Open or cystic spina bifida: this is the most serious type of spina bifida. It normally appears as a cyst on the back. Within this type of spina bifida, there are two subtypes; meningocele and myelomeningocele.
Condition prognosis
The condition can be serious, depending on size, location, and any complications involved. The higher the affected vertebrae are, the more likely the prognosis will be more serious and have more consequences. They include:
- Neurological disorders such as hydrocephalus
- Syringomyelia
- Locomotor system alterations
- Genitourinary disorders.
What are the symptoms?
Spina bifida symptoms are not the same in all patients. Some may need orthotics, crutches, or wheelchairs. Others may have urinary and intestinal problems, or even hydrocephalus. There are different types of spina bifida with different associated symptoms, including:
- Spina bifida occulta: doesn’t tend to have any obvious symptoms, although signs can be seen on the baby’s skin.
- Meningocele: the membranes surrounding the marrow push out and form a sac of fluid.
- Myelomeningocele: the vertebral canal remains open allowing the membranes around it to push out and form a sac. The nerves and tissues are normally exposed.
Tests for spina bifida
There are three tests that can be carried out during pregnancy to detect spina bifida:
- An AFP test (AFP is a protein made by the baby and the placenta during pregnancy which goes into the bloodstream) is done during the second trimester and it checks blood protein levels in the mother’s blood. This test is not conclusive. This may be done alongside human chorionic gonadotropin (hGC), estriol, and inhibin A tests.
- Ultrasounds, which can also be inconclusive
- Amniocentesis; the withdrawal of amniotic fluid from the foetal sac for analysis
To confirm spina bifida occulta after birth, certain tests will be done which may include an ultrasound, an MRI, or a CT scan.
What causes it?
The causes for neural tube defects remain unknown, however some risk factors have been identified. Risk factors include; being overweight, poorly managed diabetes, and certain seizure medications.
How can it be prevented?
Taking folic acid (which is found in most multivitamin supplements) can reduce the risk of having a baby with spina bifida.
What is the treatment?
Treatment for spina bifida depends on the seriousness of the case. In some cases treatment is not necessary.
The main type of treatment is surgery, this can be done before birth (foetal surgery), and it should be done before the 26th week of pregnancy. If left untreated, the baby’s nervous function may deteriorate after birth. Surgery can also be performed after the baby is born.
With meningocele, surgery after birth involves placing the meninges in their place and closing the vertebrae openings. With myelomeningocele, surgery is done to minimise the risk of having an infection which could leave the nerves exposed.





